Background
When in 1973, John V. Atanasoff and Clifford E. Berry were credited with their ABC computer (the Atanasoff-Berry Computer) as the first actual computer to have been created, Dr. Hubert V. Pipberger in Ohio was also using a digital computer for the automated detection of electrocardiographic waveforms.
With the help of his mathematician wife who was in charge of the library of tracings, a team of engineers and statistician Rosalie Dunn, Dr. Hubert V. Pipberger's software was applying decision tree logic and algorithms to churn out a specific diagnostic interpretation, available immediately. Dr. Ralph E. Smith, at the Mayo Clinic also worked on the subject. He introduced the electrocardiography (ECG) technicians and developed a method to store and transmit the data via satellite.
Today, varied digital diagnostic techniques record and store electrocardiograms. Furthermore, digital technology is used for coronary catheterisation, transoesophageal echocardiograms, positron emission tomography and magnetic resonance imaging. Intravascular ultrasound guides coronary intervention and digital fluoroscopy uses computerised three dimensional digital mapping for electrophysiological studies. Outpatient cardiac telemetry services such as those provided by cardionet provide real time monitoring and analysis and highly complex implantable device technologies such as the subcutaneous defibrillator, the cardiac monitor and remote monitoring.
The cardiologist has inevitably had to be familiarised with digital technology such that many of the key physicians leading the development of digital health technologies today are cardiologists – Eric Topol, for example, a cardiologist and author of the book “the Creative destruction of Medicine” and the upcoming “The patient will see you now: The future of Medicine in your hands", or Leslie Saxon, interventional electrophysiologist, whose Alive Cor (Fig 2) and Medable study will be fused in the app, to allow heart rate to be shared with a photo in the hopes to gather large-scale data from the population.
Much as how printed material has revolutionarised the way ideas were spread at the time of the Renaissance, digitised information is modifying the way we spread and collect information today. Information recorded in a binary code of combinations of the digits 0 and 1, also called bits, which represent words and images, has opened up the means we have to work, network, navigate, secure services and goods, communicate and do research.
Let's briefly explore how this new era has started to affect a patient's opportunities to control his/her health better.
1 - Patient generated data
In no area has the digital age felt more evident than with the uptake of iPads and particularly, cell phone ownership and usage - even more so than the personal computer or land lines. Today, there are nearly as many cell phone subscriptions (5 billion) as there are people (7 billion).
Apple, Google, Microsoft and Samsung have put digital health business development as a priority for 2014 and launched platforms to entice new users as well as new software and hardware developers.
Worldwide revenues from sports, fitness, and activity tracking devices are expected to be worth $1 billion in 2014 and to double within 5 years. Venture capitalists are targeting digital health for investment.
Patients have been familiar with recording blood pressure, pulse, height and weight for years but the technology now exists to transfer this information electronically directly to a doctor. Wearable technologies and smartphone devices increasingly allowing us to remotely diagnose and monitor patients.
This consumer-driven economy has produced 100,000 mobile health applications so far for download. It is unclear whether all the new developments actually meet needs that we actually may sustain but the market is working hard for us to identify new ones for us. Multiple measuring modalities of daily life with devices such as wearable sensors, cameras, data-loggers and GPS have become available.
Miniature hardware sensors allow a cell phone to track their activity, become otoscope, or take glucose readings.
The AliveCor (CA, USA) hand held ECG (Fig. 1) is a small portable device that attaches to a user's smartphone and records a high-quality single ECG.
Fig 1: The AliveCor hand-held ECG
Figure 2 describes how the products of digital technology have converged in the past 45 years. From the first cell phone, to the first computer, Internet connectivity, the sequencing of the genome and social networking. The use of the mobile connectivity of cellphones and wireless sensors and devices have created a world of shared imaging and data in health infosystems which are coordinating to "reboot" our efforts in medicine from the observation of disease to its management, prediction, and prevention; 6 characters are rebooting medicine and health, 0 and 1 for the binary digital code and A,C,G, and T, representing the four nucleotide bases of a DNA strand - adenine, cytosine, guanine, thymine.
Fig 2: Acceleration of digital technology - (Credit to Paul Sonnier and Misfit with this infographic)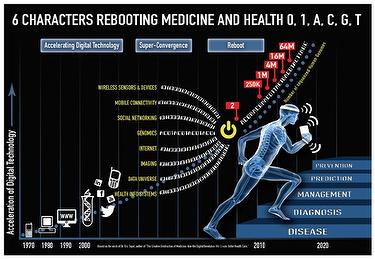
2 - Patient controlled data
Recording, storing and sharing the health-related information patients have generated is not a problem: digital health start-ups run and maintain their blogs, social feeds and other channels, websites such as “patients like me” allow easy crowd and friend sourcing with other people with similar illnesses within patient communities.
Half of all Americans have consulted the Internet for health related questions in the past year. Measuring and recording more personal health information is part of the “quantified-self” movement. A survey of users across all age groups revealed that over 75 percent want to use their own digital health technologies. Price Waterhouse Coopers reports that one in five Americans owns a wearable device and 10% use them daily. While most people buy them to help for exercise purposes they also use them to collect and track medical information.
Patients are also starting to demand greater access, involvement and control of their own medical and personal data. Electronic health records as opposed to medical health records, may give patients access to information from all the clinicians involved in their care. Microsoft health vault, dossia are examples of person-centred health records, or patient portals, allowing patients to upload their health data onto customisable, editable platforms enabling them to share their medical history with the health professionals of their choice. Network connectivity is improving and cloud storage is becoming more affordable, patients might be able in the near future to maintain their own databases containing their medical notes as well as their medical images, x-rays, cross sectional images and ultrasounds, with links into external discussion sites with potentially their own forum. In another social media site, the LinkedIn group “Digital Health” headed up by Paul Sonnier has grown in five years to a community of over 30,000 digital health professionals. Discussions help shape the announcements, developments and funding of innovative digital health technologies.
3 - Forming communities, seeking professionals and online video consultations
With patient data, images and clinical information stored on the Internet, technologies are now developing that allow us to consult with our patients using network video. It is already possible to use Facetime or Skype for such services. Patients can choose to have a consultation with the physician of their choice at a time that suits them from the comfort of their home. Convenient secure online systems allowing patients to get instant access to medical advice but accessible tools such as skype might also get wide-spread medical use, as this hospital in England has decided to start using.
Smartphone based software such as Babylon (Fig. 3) and HealthTap might have the same effect on face-to-face medical consultations that online retailing has had on shopping. Why would empowered patients who control their own data wait to consult with their local specialist when then can choose the one that they want, anywhere in the world, at a time that is convenient for them? We are talking about 24/7 availability of networked world access to medical advice, using high quality medical and nursing specialists over online video technologies.
The island of Jersey has recently become the first community in the world to have this technology funded by the government.
Trusted websites such as “patients like me” can direct patients to new doctors. They are online social sites for patients to share information, discuss cases and identify new treatments and specialist physicians.
Some websites have taken this one step further and provide online rating systems for physicians such as healthgrades, rateMDs or vitals.com so that future patients can read reviews of practice by other users instead of relying on the peers of their providers for advice.
4 - Implantable device technologies and remote monitoring
Devices such as implantable electrogram loop recorders and injectable monitors, patch biosensors allow patients to choose the type of information they wish to record. Community care and patients with chronic diseases are starting to benefit from home digital health technologies that can track and map clinical parameters, highlighting to their physician or caregiver when parameters change. A number of different telehealth - remote collection of patient data - and telecare - remote monitoring - (see e-journal article remote monnitoring for pacemakers here) pilots are underway to determine if these systems can keep people at home - reducing hospital admission and improving patient outcomes, particularly in chronic heart failure, diabetes and chronic obstructive pulmonary disease. Some novel community services such as the Call and Check service are de-medicalising care further, with visits and checks provided by postmen.
Concerning the AliveCor recordings, these are stored in the user’s cloud account or linked to their doctor’s account. ECGs can be remotely analysed, emailed or printed for clinical interpretation. The software now also has an FDA approved algorithm for the detection of atrial fibrillation. This type of technology allows a rapid diagnosis for patients with symptoms of palpitation that would otherwise need prolonged monitoring with Holter ECGs and event recorders. It also allows for more remote follow-up of patients with complex arrhythmias who can discuss their symptoms over the telephone or Internet whilst sharing their traces directly with their electrophysiologist. Another interesting technology is handed by Proteus, which offers a pill, that much like a potato battery, can track whether a patient takes his medicine or not. Vital sign monitoring is also accessable from remote locations.
5 - Application derived diagnostic algorithms, genomics and big data
High powered computing systems such as IBM’s Watson – initially developed by IBM to play the Jeopardy game, a new challenge after its victory of Deep Blue against G. Kasparov in chess – are starting to analyse the “Big Data” that these and established clinical devices are generating, potentially allowing computers to start providing more accurate diagnostic advice and early warnings of impending clinical deterioration. Leslie Saxon's hope is for all the cellphones of the world to gather information that can be used in a population-wide study. The Personal Genome Project (PGP) is a cohort study to sequence and publicie the complete genomes and medical records of 100,000 volunteers along with their medical records, various measurements, MRI images, etc (evidence of their phenotype). All data will be placed within the public domain and made available over the Internet so that researchers can test various hypotheses about the relationships among genotype, environment and phenotype as well as potential discrimination by insurers and employers in the event of results showing a predisposition for diseases. As sequencing technology becomes cheaper, and the societal issues mentioned above are worked out, it is hoped that one day every person will have access to his or her genotype to be used for personalised medical decisions. Recruiting is ongoing in the US and will be opening up to Europeans shortly.
Craig Venter was one of the first to sequence the genome. His talk on the biological-digital converter discusses digitising biology, following his discovery of how synthetic genome successfully instructed the cell to create living proteins.
Pharmacogenomics will improve the safety and precision of prescription medications. Routine molecular biologic digitisation of humankind is around the corner, he says.
Sequencing is already making a difference in cancer treatment as it offers the possibility to analyse the specifics of the patient and their disease. (For an e-journal look at genetic testing in cardiomyopathy, look here).
6 - Online medications
Drug prescriptions and deliveries remotely without direct physician input based on patient data and world access to medical advice. A 24/7 availability of networked, high quality medical and nursing specialists using online video technologies.
7 - Medical education
Streamed, live cases with interactive discussion with clinicians. Online case reviews and advice. Worldwide access to peers and new opinions. Active participation in online curation of public health information is starting to be promoted – for example medical schools are to offer credit for offering medical editing on Wikipedia. Patients have been familiar with recording blood pressure, pulse, height and and weight for years but the technology now exits to transfer this information electronically directly to a doctor. Wearable technologies and smartphone devices are increasingly allowing us to remotely diagnose and monitor patients.
Fig 3: The health app free to download with an option to pay as you go for consultations with GPs or consultants, or subscribe annually (UK). 
Key impacts
Here again are the 8 key impacts of digital health evolution on cardiology practice
- Patient generated data: Health trackers and devices that allow patients to collate their own independent health information for feeding into patient controlled data.
- Patient controlled data: Online patient portals allowing patients to store and curate (gather, collect) their data whilst controlling who can view their health data.
- Forming communities, seeking professionals and online video consultations: convenient secure online systems allowing patients to get instant access to medical advice.
- Implantable device technologies and remote monitoring: Devices such as implantable electrogram loop recorders, injectable monitors, patch biosensors allowing patients to choose the type of information they wish to record for patient-generated data.
- Application derived diagnostic algorithms, genomics and big data: Complex software algorithms providing medical diagnosis based on information provided by items 2 and 4 - patient controlled data and implantable device technologies, the study of our genes and big data derived from masses of patient generated data.
- Remote monitoring and diagnosis: Wearable or insertable device technologies that transmit to health professionals for continuous monitoring and analysis.
- Online pharmacies: Drug prescriptions and deliveries remotely without direct physician input based on patient data and application derived diagnostic algorithms, genomics and big data.
- Medical education: Streamed, live cases with interactive discussion with clinicians. Online case reviews and advice. Worldwide access to peers and new opinions.
Conclusions
Our practice has benefited from what the digital age has brought to us: digital diagnostic tools, electronic medical records, ambulatory and remote recordings, online education and application derived diagnostic algorithms. On the other hand we are seeing patients collecting their personalised data, choosing among practitioners according to reviews, getting informed on their treatment options, networking with their peers and deciding whether to consult on-line or not, having devices implanted into their bodies/skin, choosing the information that is recorded and sent remotely, as well as order medication, form communities and seek advice and education online.
Patients can be very proactive in their health if they so choose. Today, only the most motivated patients upload their data. One can expect that in the future all patients will have their data uploaded automatically via local network to a single patient file.
Some cardiologists have embraced these changes as a vital part of patient and community engagement, others are reluctant. Valentin Fuster in a Nature editorial review wrote: embrace with open and inquiring minds what could become the 'future' of medicine. In our health conscious world of wellness, digital health can help modify peoples’ behaviour to bring about health benefits by offering information into their data that is motivational and achievable to steer people to longer and healthier lifestyles. We will also benefit from from more personalised information via the genome and pharmacogenomics while also getting broader evidence medicine from population wide observational studies.
The digital age has empowered both cardiologists and patients alike. We might need to modify our practices though, by paying attention to reviews on online rating, using scriptpads to avoid medical error, embracing patient involvement and keeping abreast of new technologies and advances in the area of genomics. Today's computer technology has produced microprocessorsand is trying to create artificial intelligence as Siri can attest to. Big data and personalised medicine might let physicians feel like the shift of power has gone to statisticians and geneticists, in addition to the newfound power of motivated patients. Today patients ask their doctor. Tomorrow they may ask their data.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.