Background
Endurance athletes commonly exhibit larger cardiac dimensions than the rest of the athletic population, with cardiac enlargement representing a physiological adaptation to intensive training(1). However, relevant enlargement of the aorta cannot be considered a common consequence of the athlete’s heart, with aortic dilatation being associated with an increased risk of adverse aortic events(2).
Risk factors for aortic dilation include advancing age, male sex, large body size, hypertension (particularly if not controlled), genetic syndromes including bicuspid aortic valve (BAV), connective tissue disorders, such as Marfan Syndrome(3,4).
Aortic root dilation is the leading cause of aortic insufficiency, whereby the aortic valve does not provide adequate closure to prevent regurgitation of blood from the aorta into the left ventricle. Aortic root dilation can also lead to aortic dissection because increased wall forces in the area of dilation lead to a tear in the aortic wall that can extend retrograde into coronary vessels or anterograde into the ascending and descending aorta.
Introduction
We present a case of a 42-year-old practicing competitive cycling and running for 8 hours per week. He was admitted to our Center for Sports Cardiology for a complete clinical assessment, including physical examination, resting ECG, ambulatory ECG monitoring, and transthoracic echocardiography (TTE) because of uncommon premature ventricular beats (PVBs) during the recovery step of an exercise testing performed for pre-participation screening. The athlete has no relevant prior medical history, no cardiovascular risk factors, or syncope. Family history was negative for coronary artery disease or sudden cardiac death. Physical examination was normal, and 12-lead ECG revealed common training-related findings, including bradycardia and incomplete right bundle branch block. The echocardiographic examination was performed according to the current standards(5).
How should we enquire about aortic root diameter measurement?
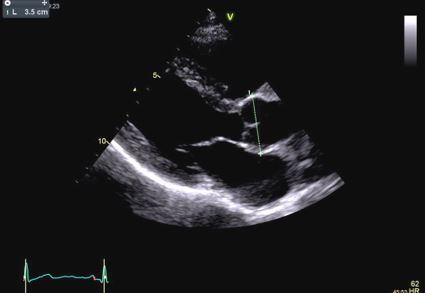
Aortic root diameter measurement should be performed in adults (>15 years) from the parasternal long-axis view during diastole using the L-L convention, preferring 2D measurements (Figure 1)(6).
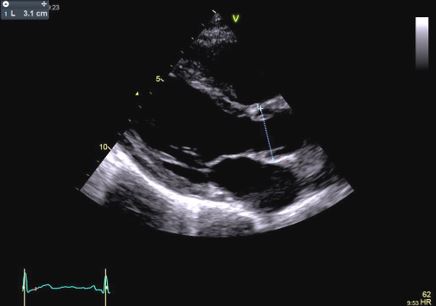
In children and individuals under 15 years, aortic root diameter measurement is best measured in parasternal long-axis views during early to mid-systole, using the inner edge-to-inner edge technique (Figure 2)(7).
What is the upper limit of normal aortic root diameters in competitive athletes?
In several large cohort studies, the upper limits of physiologic remodeling of the aortic root have been reported to be 40 mm in male athletes and 34 mm in female athletes(8,9). However, parameters of aortic root diameter are also thought to be proportionate to anthropomorphic variables, such as height, body size, age, and sex. Height appears to be one of the most significant determinants of aortic root size(10,11). To avoid the confounding effect of body size and age, the z-score has been proposed, particularly for children(12). The z-score describes how many standard deviations above or below size or age-specific population mean a given measurement lies(13).
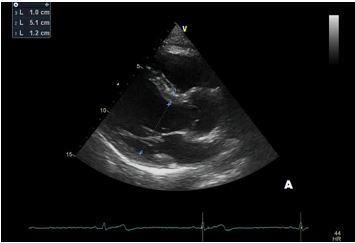
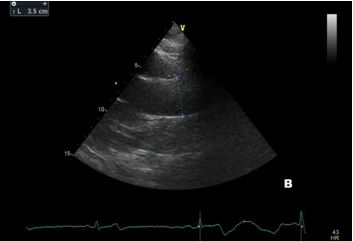
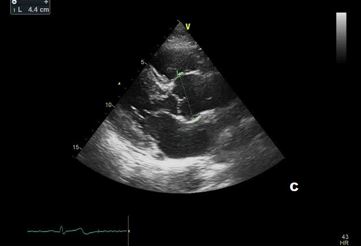
In our patient transthoracic echocardiography revealed normal diameters of the left ventricle with mild septal hypertrophy (EDD: 51 mm; ESD: 31 mm; IVS: 12 mm; PW 10 mm) with mild enlargement of the right ventricle (mid-cavity diameter: 37 mm), with normal biventricular systolic function. However, TTE revealed a tricuspid aortic valve with dilatation of the aortic root (44 mm, Z-score >2: Z=4.2). Ascending Aorta and aortic arch diameters were normal in absolute values (35 mm and 32 mm, respectively) and when keeping into consideration body size.
Management
According to the current guidelines, an exercise test with an assessment of blood pressure response is recommended before engaging in sports(14). We performed cardiopulmonary exercise testing. Blood pressure response was normal during the test, and a normal functional capacity was demonstrated. The test confirmed the presence of PVBs, with a left bundle branch block morphology. The ambulatory ECG monitoring showed rare, isolated PVBs with the same morphology. An abdomen ultrasound revealed a normal diameter of the abdominal aorta.
Athletes with normal left ventricle size and function, with no arrhythmia at rest or under exercise stress test, could undertake all sports, as long as mild aortic regurgitation; while athletes with moderate aortic regurgitation, aortic root <43 mm and normal LV size and function may engage in moderate-intensity sport (15). In our case, aortic dilatation was not associated with an aortic regurgitation or stenosis. However, aortic root was significantly dilated and, according to the current national and international recommendations, the athlete was disqualified from sports competitions, and a personalized physical activity was prescribed, avoiding high-intensity exercise and contact sports(14). As per protocol in our Center, the first clinical re-evaluation was performed after 6 months. Resting ECG was normal, and TTE revealed a stable aortic root diameter.
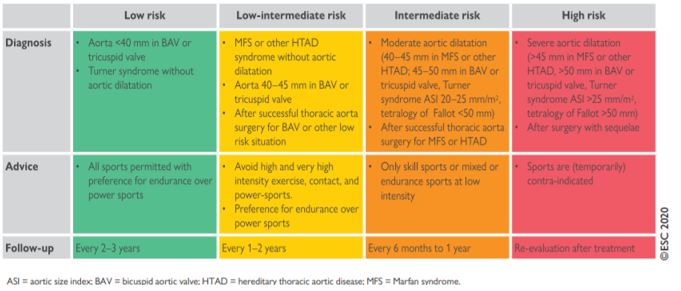
What is the risk of performing sports in patients with aortic pathology?
Competitive sports, especially those involving high-intensity activity and frequent collisions (such as boxing, bodybuilding, and gymnastics), are particularly risky for patients with more-than-mild aortic root dilation because they are thought to increase the risk of aortic dissection and rupture(16,17). In contrast, sports with low static and dynamic components are safer and less risky (Figure 3). According to the ESC guidelines, the patient was considered a low-intermediate risk. It was recommended to avoid high and very high-intensity exercise contact, with the preference for endurance over power sports(14). The first evaluation was scheduled after 6 months, and then a yearly follow-up was then established to monitor aortic root diameter.
Follow up
After a year, our patient underwent TTE that showed an aortic root dimension of 44 (Figure C), stable in comparison with the previous evaluation, with no modification of ascending aorta measurement and no LV enlargement (Figure A and B). He continues with yearly follow-up, continuing with personalized physical activity previously prescribed.
Serial echocardiography is recommended at least once a year for asymptomatic patients with mild-to-moderate aortic dilation(18). In patients with associated aortic regurgitation, the frequency of serial echocardiography depends on the severity of valvular regurgitation, level of systolic function, degree of (LV) dilation, and whether previous serial studies have revealed progressive changes in LV size or function(18).