Carriers of pathogenic or likely pathogenic (P/LP) variants in the desmoplakin (DSP) gene are prone to experiencing inflammatory, myocarditis-like episodes, a key phenotypic feature of DSP cardiomyopathy. These episodes are relatively common, affecting around 15% of patients. This clinical finding underscores that DSP cardiomyopathy is an inherently fibrotic and inflammatory form of cardiomyopathy.1 Recent data suggest that immunosuppressive treatment of these episodes could significantly improve the clinical course.2 Nevertheless, specific immunosuppressive protocols for this condition are missing. In the following lines we will try to shred some light on this controversial topic.
Despite the recent 2025 ESC Guidelines on Myocarditis and Pericarditis mention the presentation of myocarditis with a potential genetic background there is no specific recommendations for diagnosis and treating myocarditis explicitly linked to DSP variants. General guidance recommends clinical risk stratification to guide work-up at admission and identify cardiogenic shock, NYHA III-IV, extensive fibrosis, or new-onset severe systolic dysfunction as well as sustained ventricular arrhythmias or high degree AV block as high-risk clinical scenarios. In this cases, endomyocardial biopsy (EMB) should be considered to establish a definitive diagnosis and guide aetiology-specific treatment Whether these general recommendations should be followed for patients with known DSP variants is not clear and maybe EMB could be considered only for fulminant or discordant phenotypic presentation. 3
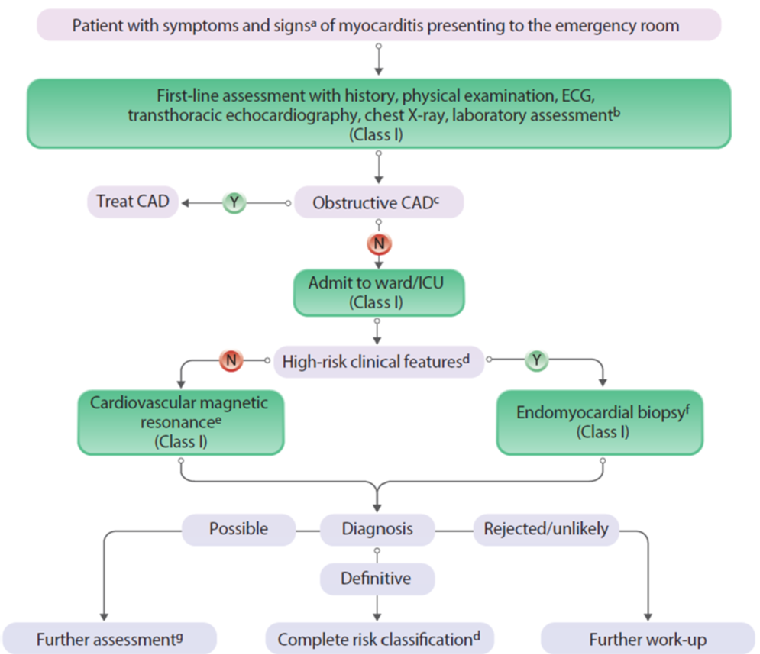
Modified from Figure 5 Diagnostic algorithm and triage for inpatient myocarditis. Extracted from 2025 ESC Guidelines for the management of myocarditis and pericarditis. Schulz-Menger et al. 2025 d Cardiogenic shock, NYHA III-IV, extensive fibrosis, new-onset severe systolic dysfunction, sustained ventricular arrhythmias or high degree AV block.
As a general framework, pharmacological treatment of virus-negative inflammatory cardiomyopathy could provide some guidance in the absence of specific clinical evidence. Overall patients with fulminant episodes of cardiogenic shock should received high dose bolus of methylprednisolone (7–14 mg/kg/day; ie: 500-1000 mg for a 70 kg patient) for 3 days followed by tapering whereas patients with milder presentations could benefit from 1 mg/kg/day p.o. dosing. In patients with persistent inflammation, adding a second immunosuppressant such as azathioprine, mycophenolate, cyclosporine or methotrexate might be considered.3
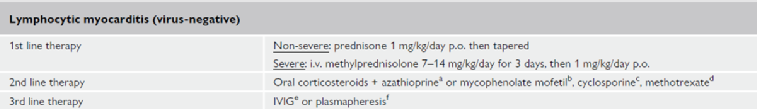
Modified from Table 12 Therapy for specific forms of myocarditis. Extracted from 2025 ESC Guidelines for the management of myocarditis and pericarditis. Schulz-Menger et al. 2025
While the ESC guidelines recommend to defer on implantable cardioverter-defibrillator (ICD) placement during the acute phase of the disease, the threshold for ICD placement should be lower in ARVC in cases of primary prevention including DSP variant carriers.3
The recent retrospective analysis by Gasperetti et al., leveraging data from the DSP-ERADOS network provide also relevant information about pharmacological treatment of these patients. I this cohort, 177 carriers of DSP variants who suffered myocarditis-like episodes at any point of their clinical history were identified and treated according to clinical judgement of attending physicians. In this cohort, 31.6% of patients received immunosuppression for their first episode, while 18.1% were treated using nonsteroidal anti-inflammatory drugs (NSAIDs) or colchicine. The remaining 50.3% of patients did not received treatment at the time. 2
Despite treatment with NSAIDs or colchicine did not appear to influence subsequent ventricular arrhythmias or heart failure outcomes, patients treated with immunosuppressive medications experienced significantly lower rates of VA [1.8%/y versus 8.3%/y; HR 0.18 (95% CI, 0.07–0.45); P<0.001] and HF hospitalizations [0.7%/y versus 5.5%/y HR 0.09 (95% CI, 0.02–0.39); P=0.001]. The most common regime involved corticosteroids as a single agent or combined with other agents such as azathioprine or mycophenolate.2
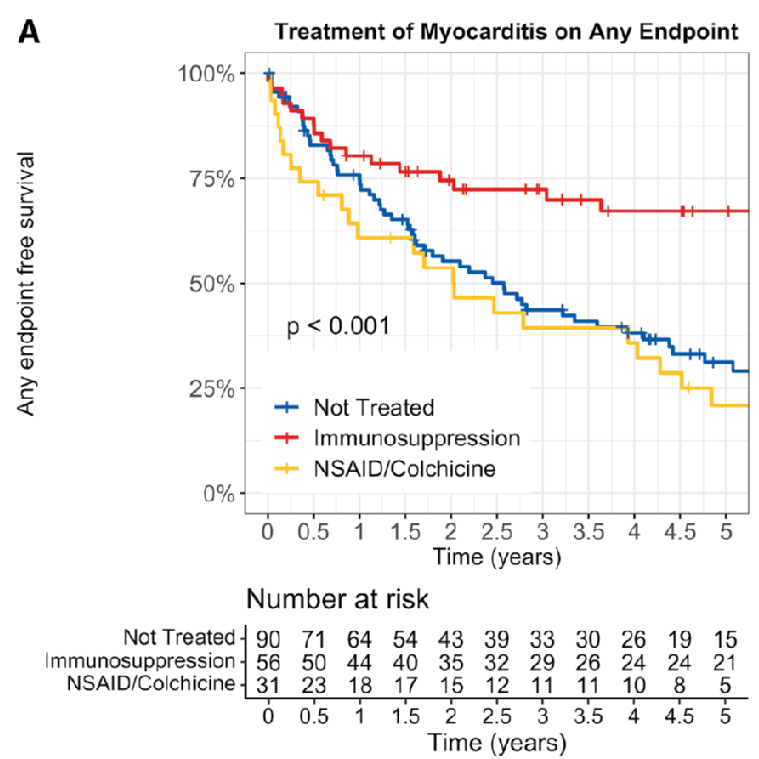
Survival free of ventricular arrhythmias or heart failure episode in DSP carriers presenting with myocarditis-like episodes according to immunosuppression regime. Extracted from Prognostic Role of Myocarditis-Like Episodes and Their Treatment in Patients With Pathogenic Desmoplakin Variants. Gasperetti et al. 2025
Crucially, because these data are based on retrospective analysis where treatment decisions were heterogeneous, they are hypothesis-generating and strongly support the need for future prospective evaluation, including randomized controlled trials. Such studies are necessary to definitively confirm the therapeutic benefit of immunosuppression, evaluate the efficacy of individual agents and dosing protocols, and further investigate the genetic mechanisms driving recurrent inflammation.

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.