Unrecognised myocardial infarction has relevant prognostic implications. To detect these necrotic areas a cardiologist has very powerful technology at hand : gadolinium late enhancement MRI which has excellent diagnostic accuracy.
In a recently published paper (1), it has been pointed out that areas of myocardial scar has been found in an unexpectedly large number of patients referred to a cardiologic environment for symptoms or signs of ischemic heart disease. This result is not that surprising, as it is well-known that at least 25% of Q-wave myocardial infarction (MI) are clinically unrecognised (2).
The prevalence of myocardial scar is probably even higher if one considers the number of unrecognised MI and the low sensitivity of ECG (Fig 1), namely on non Q-wave MI. However, this paper leads to two further relevant considerations:
The prognosis of patients with unrecognised MI is severe (45%-55% of mortality within 10 years)(1, 3)
The possibility of confirming/excluding the presence of intra-myocardial scar with an accurate and almost risk-free methodology such as gadolinium late enhancement MRI, which has shown an excellent diagnostic accuracy (1)
The capability of detecting the presence and location and of evaluating the necrosis quantitatively does not require sophisticated MRI equipment nor particular levels of knowledge, since the technological requirements for obtaining good quality images are today part of standard multipurpose scanners. Furthermore, the “black and white” (black being he normal/viable tissue and white the necrotic one) appearance of the images at the level of myocardium allows for intuitive interpretation and is relatively easy to perform (see Fig 2). Moreover, standard cardiac MRI examination gives a comprehensive and reliable evaluation of cardiac morphology, of bi-ventricular function, of scar detection, etc.
Fig 1: ECG shows no significant abnormality.
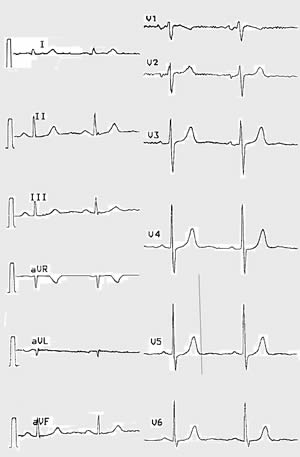
ECG from a 50 year old woman with aspecific symptoms and no history of previous myocardial event. The ECG shows no significant abnormality.
Fig 2 Evidence of unsuspected myocardial scar - in the same patient -at the level of inferior wall of left ventricle with Gadolinium late enhancement MRI.
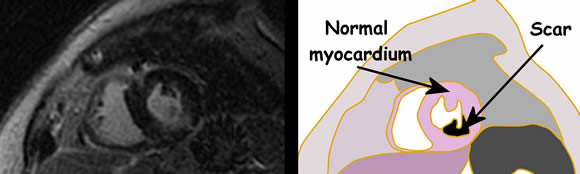
Magnetic Resonance image (delayed T1 gradient Echo after Gd-base contrast administration) in short axis of the heart from the same patient of Figure 1. There is evidence of unsuspected myocardial scar at the level of inferior wall of left ventricle. The patient then underwent invasive angiography which showed a three vessel disease and namely an occluded right coronary artery.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.
Conclusion:
From the above-mentioned data, it results that the clinical cardiologist would have to consider an extensive use of this imaging approach because it is progressively shown to be a highly cost/effective imaging tool which is already available in most hospitals of the western countries. The implementation of the other imaging techniques already in use with a full integration of MRI will indeed become a major goal in the very next future.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.