Viral myocarditis : clinical manifestations are varied
Clinical manifestations of myocarditis are extremely varied, - they range from an asymptomatic state, to fulminant acute heart failure, and can also be conduction disturbancies, or ventricular tachyarrhythmias (1), and even be a global biventricular dysfunction (2).
A number of agents induce myocarditis. Among them, viruses are believed to be the most common agents causing myocarditis in developing countries (3).
- 1st phase : the acute phase : entry and proliferation in the myocardium of the causative virus
The acute phase of the disease is triggered by the entry and proliferation in the myocardium of the causative virus. This phase concludes with the activation of the host immune system, which attenuates viral proliferation but may also enhance viral entry.
Ideally, the immune system should downregulate to a resting state once viral proliferation is controlled. However, if host immune activation continues unabated despite elimination of the virus, autoimmune disease may result, initiating the second phase of the disease.
- 2nd phase : a dilated cardiomyomathy develops
T cells may then target the host’s own tissue through molecular mimicry. Cytokine activation and cross-reacting antibodies may further accelerate the process (4). Chronic inflammatory and dilated cardiomyopathy are a common evolution of the disease (5). Some remodeling mechanisms leading to dilated cardiomyopathy may be specific to myocarditis.
Badorff and Knowlton (6) have shown that a coxsackieviral protease can directly modify the sarcoglycan complex in myocytes. This may provide one of the potential mechanisms explaining the significant ventricular dilatation that may be seen soon after viral infection. Persistent myocyte viral gene expression, after infectivity has passed, might be another cause of progressive dilated cardiomyopathy. Cytokines may also contribute to the development of dilated cardiomyopathy. In addition, viruses may directly cause myocyte apoptosis. Ongoing viral persistence is associated with a much worse outcome such as early death or a required transplantation (7).
CMRI : added benefits
Cardiac magnetic resonance imaging (CMRI) can characterise tissue to a greater degree than other imaging modalities and can detect focal or global inflammation (8).
How it detects myocarditis CMRI is the result of different magnetic relaxation times, T1 and T2 which are different in various tissues. The tissue T2 relaxation time is an indicator of tissue water content, which is increased in inflammation or necrosis, i.e. during early myocardial infarction or myocarditis. Gagliardi et al [9] were the first to publish a case series on the use of CMR for non invasive diagnosis of acute myocarditis in eleven children and infants. Compared with biopsy, T2-weighted spin echo CMRI sequences were found to have a 100 % sensitivity and specificity.
CMRI and early detection of myocarditis infection : the STIR sequence detects edematous tissue
We examined consecutive patients who were presented with symptoms of fatigue, weakness and/or palpitations after respiratory tract infection but normal left ventricular function with a special T2-weighted sequence (also called STIR sequence). We found an elevated signal intensity of the myocardium indicating edematous tissue which may be the first step in the development of myocarditis (10).
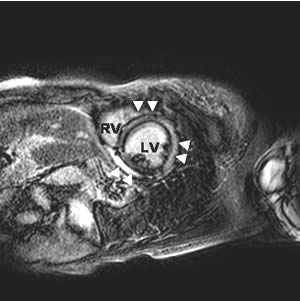
Fig 1 : An example of T2-weighted (STIR) image of a patient showing an enhanced signal intensity. This indicates myocardial edema.
LV: left ventricle. RV: right ventricle.
▲▲: elevated signal intensity of the myocardium
↑↑: small pericardial effusion

Figure 1 represents an example of a female patient with enhanced T2-weighted image indicating myocardial edema. The patient had dyspnoe and ventricular premature beats after a respiratory tract infection.
CMRI and myocardial viability : hyperenhanced, i.e. white areas reveal altered myocardium
Reports of imaging myocardial injury using T1-weighted pulse sequences after administration of intravenous gadolinium have been known since the mid 1980s. In the landmark paper of Kim et al (11) the usefulness of delayed enhancement imaging was thoroughly investigated.
After a intravenous bolus of a paramagnetic contrast agent, e.c. gadolinium T1-weighted pulse sequences are performed after 10-15 minutes. Normal uninjured myocardium shows a black image. Hyperenhanced, i.e. white areas reveal altered myocardium. This technique has been shown to be effective, in both animals and humans, in identifying the presence, location, and extent of acute and chronic myocardial infarction. I
n addition, hyper-enhanced myocardial regions can be visualised in patients with hypertrophic or dilatative cardiomyopathy (8). In myocarditis delayed contrast-enhanced cardiac magnetic resonance has been thoroughly investigated (5,12). A typical subepicardial late contrast-enhancement is highly predictable of myocarditis in suspected patients (12) (figure 2).
Figure 2 : The delayed contrast enhanced image of the same patient showed diffuse hyperenhanced areas in the typical midmyocardial location (▲▲).
LV: left ventricle. RV: right ventricle.
Diagnostic approach in patients with suspected myocarditis. Biopsy is unsuited – unsensitive and invasive.
An autopsy series of consecutive cases have demonstrated an incidence of myocarditis at approximately 1 % (12). On the contrary, myocarditis is seriously underdiagnosed clinically. The gold standard has been myocardial biopsy traditionally. However, it is generally specific but insensitive for clinical use, mostly because of the focal nature of the disease. In addition, in ambulant patients with normal left ventricular function the risk of this invasive procedure is not to be underestimated and is not accepted by the majority of patients.
Thus, non invasive approaches to detect myocarditis are necessary. The traditional diagnostic tools are ECG, laboratory values, especially troponin T or I, creatine kinase and echocardiography.
In summary, cardiac magnetic resonance imaging should be performed in patients with suspected myocarditis, e.g. after a gastrointestinal or respiratory tract viral infection and symptoms of fatigue, weakness and/or palpitations to confirm or to rule out the correct diagnosis whereas myocardial biopsy is unsuited because of its insensitive and invasive nature.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.