Left and right ventricular volumes, mass and regional function
Despite continuous improvements in echocardiography, CMR remains the reference standard for the assessment of left and right ventricular volumes, mass and regional function. This is due to its superb contrast between blood and myocardium as well as its uninhibited 3D view.
In most patients assessment with echocardiography is fully sufficient, however, difficult patients (e.g. with suboptimal echocardiographic image quality, or complex decision making in mitral or aortic regurgitation) will profit from the more accurate quantification and give a stronger stand for more aggressive therapy (e.g. ICD implantation).
Most patients can be followed up with echocardiography, however, if exact numbers remain important e.g. to postpone surgery (e.g. mitral insufficiency) and detect smaller changes during follow up (e.g. due to therapy) CMR should also be used for follow up.
Fibrosis
In the last years a technique called “late enhancement” or “late gadolinium enhancement” has opened up a range of strong indications for CMR (1).
Contrast agents, which are routinely used for MR imaging diffuse from the vessels into the interstitial space, but not into the cell itself. If cell membranes are ruptured (as in acute myocardial infarction) of the interstitial space is enlarged (as in inflammation or fibrosis) the contrast agent concentration increases causing enhancement in the MR images. This technique has been extensively validated in animal experiments and patient studies(2, 3).
Due to its higher spatial resolution, MR images show the location and transmurality even of small myocardial infarctions (figure 1), which are currently missed by other techniques, such as SPECT or PET.
Enhancement can be found in acute and chronic myocardial infarction, many patients with dilative cardiomyopathy, longstanding hypertrophic (obstructive) cardiomyopathy and myocarditis. Similarly enhancement can be found in patients with storage disease. The typical patterns are described in figure 2 (4).
A remaining difficulty is the differentiation between patients with previous myocarditis and patients with dilative cardiomyopathy, since both may have a similar pattern of fibrosis (midwall striae) (5). It is possible, however, that some patients currently classified as dilative cardiomyopathy may actually be patients after destructive myocarditis.
Within one CMR examination a number of different questions can be answered:
- Ventricular volume
- Stroke volume
- Ejection fraction
- Wall thickness and thickening
- Valvular function
- Regurgitant volume
- Fibrosis (amount, transmurality, underlying etiology)
If these questions can be adequately solved with echocardiography, the underlying etiology can be determined and a more exact quantification is not needed, MR imaging is not required. However, if open questions remain, CMR helps to answer these questions and, thus, optimally guide therapy.
Figure 1
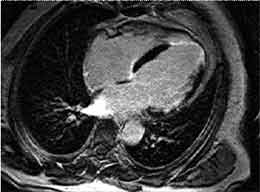
4-chamber view with the late enhancement technique in a patient with myocardial infarction. Ten minutes after contrast agent injection normal myocardium remains black, whereas fibrosis enhances due to the accumulation of contrast agent in the enlarged interstitial space. Note the transmural infarction in the apex and the subendocardial pronounciation of the infarction in the lateral wall.
Figure 2
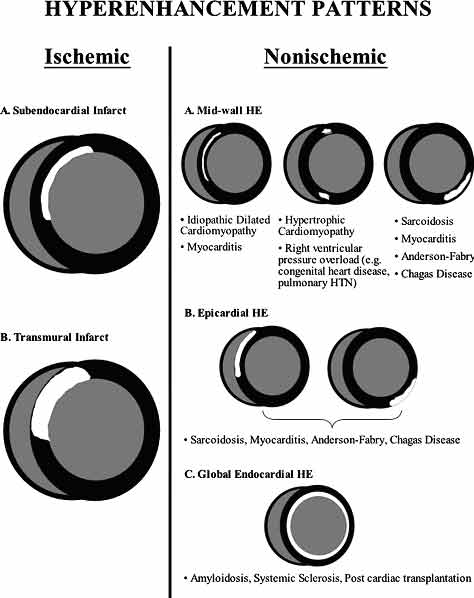
Typical enhancement patterns in patients with ischemic (left) and nonischemic (right) etiologies of myocardial fibrosis. (From Mahrholdt et al, Eur Heart Journal 2005).
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.