This report summarises the main electrocardiographic findings related to the “athlete’s heart”. Although the ECG may also help to detect some subjacent cardiac disorders related to malignant arrhythmias or sudden death in patients performing sport practice (Wolff-Parkinson-White, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, long QT syndrome), this review will focus only on the electrocardiographic variants of previously healthy sport practionners, and, thus, on the electrocardiographic changes induced by the physical training itself.
I - RHYTHM DISORDERS
A) Sinus rhythm disorders
Moderate and asymptomatic sinus bradycardia (HR 40-50 bpm) is the most common disorder in sport practioners (Fig. 1). It is due to neurovegetative changes related to training (parasympathetic predominance), and its prevalence is especially high in high-level aerobic resistance sports (cyclists, marathon runners, skiers,...), occuring up to 50-100% of patients [1;2]. Severe bradycardia (HR < 35-40 bpm) is rare, although it can be present in older sport practioners (> 40 years old) and preferably at nighttime. Irrespective of the baseline heart rate, sinus bradycardia is considered benign if the patient remains asymptomatic and a normal increase in heart rate is observed during exercise; in especially severe cases, a stress test is recommended [3].
Sinus arrhythmia is frequent (up to 15-20% of athletes), and so are sinus pauses that last longer than 2 seconds (up to one third of patients [2;4]), whether at night or during the day. When the baseline heart rate is low, it is possible to find a competing nodal rhythm (0.5-2.5% of patients [2]) or an ectopic atrial rhythm (13.5-69% of patients [4]). Again, these findings are not worrying if normal sinus rhythm appears during exercise (Fig. 2).
B) Conduction disturbances
In about 2% of sport practionners’ endurance ECGs, it is possible to find long P waves, sometimes bimodal, probably related to interatrial conduction disturbances. These findings, however, are not associated to changes in atrial size measured by echocardiography [2]. Intraventricular conduction disturbances are thought to be due to an increase of ventricular mass, and preferably affect the terminal portions of the right bundle-branch (right ventricle dilatation). In these cases, the ECG can show an incomplete right bundle-branch block or notched-R waves in inferior leads and in precordial V1-V2 leads. Complete bundle-branch block is not common in athletes’ ECGs. Left bundle-branch block is extremely rare and not attributable to sport practice itself, while right bundle-branch block seems to be present in the same proportion as in the general population, although some controversial results have been obtained in high aerobic resistance athletes [2;5;6].
Atrioventricular conduction disturbances are frequent in sport practioners’ ECGs. First-degree AV block is the most common finding, followed by Mobitz type-I second-degree AV block. The prevalence of first-degree AV block in a baseline ECG is approximately 7-10% [4;5]. However, when a 24-hour Holter is performed, it can be observed in up to 27.5-40% of patients, while type-I second degree block can be present in 15-22% of patients [1;2;7]. Both are secondary to parasympathetic hypertony, and are especially common among high aerobic resistance athletes. Both are benign conditions, and must disappear during exercise or hyperventilation (Fig. 3).
More severe AV conduction disturbances are rare. Episodes of Mobitz type-II second-degree block and less frequently third-degree block may be present in some high-level athletes at night (24-hour Holter), but if present in baseline ECG during the daytime, structural heart disease or other subjacent conditions should be ruled out, especially if the disorder does not disappear during exercise.
C) Other arrhythmic disorders
Atrial or ventricular premature beats are not usual in the ECG of sport practionners but can be present in some cases (diving). Their prevalence is about 1.5% and typically disappear during exercise [2].
In the last years, a relation between a long-lasting sport practice and the developement of atrial fibrillation has been established [8-10]. In a study with 51 patients with atrial fibrillation and 109 controls, the practice of more than 1500 hours of sport during a lifetime appeared as the threshold for this association [8]. These results are parallel to those observed in a study with top ranked orienteers [9] and in another study with marathon runners (personal data). Adjusted to age, body mass index and blood pressure, marathon runners present 12.9-fold risk of developing atrial fibrillation.
Sudden death may occur during sport practice, but always in the setting of subjacent proarrhythmic disorders, like Wolff-Parkinson-White, hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, long QT syndrome and, less frequently, the Brugada syndrome. The ECG may be useful to identify these disorders, which are not secondary to sport practice itself and thus, not specifically treated in this review.
II - CHANGES IN VOLTAGE
It is very frequent to find high-voltage QRS complexes in the athlete’s ECG (Fig. 2), although only 12% of recordings show clear electrocardiographic signs of left ventricular hypertrophy [2]. However, the correlation of these ECG findings and the echocardiographic measures of ventricular wall thickness seems to be very low (10%-50% depending on the series), being the Sokolow’s index the best correlated parameter in different publications [6;11;12]. In fact, in a study with 947 highly trained athletes, only 1.7% had wall thickness greater than or equal to 13 mm, and thus, compatible with the diagnosis of hypertrophic cardiomyopathy [13].
QRS complexes are larger in those athletes practising highly dynamic sports requiring high cardiovascular work (decathlon, cyclism, rowing), in whom electrocardiographic criteria of left ventricular hypertrophy are found in 29% of participants. Other sports with medium (swimming, rugby, skating) or low (bowling, golf) cardiovascular demand present electrocardiographic signs of hypertrophy in only 12.3% and 5.4%, respectively [2]. In women, QRS complexes usually have normal voltage, electrocardiographic hypertrophy being extremely rare.
III - CHANGES IN REPOLARISATION
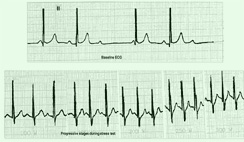
The most common finding is the presence of an early repolarisation pattern, consisting in ST-segment elevation (with upward concavity in its initial portion), elevation of J-point (up to 3-4 mm in precordial leads) and high symmetric positive T-waves, widely distributed in the ECG [14]. This pattern can be observed in up to 60% of ECGs performed in elite athletes [2], and must be distinguished from other conditions that also present with ST-segment elevation, such as acute myocardial infarction or the Brugada syndrome (Fig. 4). Typically they disappear during exercise. Vagotonic T-waves are also frequent (high narrow positive T-waves, Fig. 1 and Fig. 4), and can be present without an early repolarisation pattern in up to 15% of patients [2]. They disappear when physical training is stopped.
In some cases, especially in high aerobic sport practionners, asymmetric negative T waves appear from leads V1 to V4 (Fig. 5). Although also explained by vagal hypertony, they may resemble those present in some myocardiopathies, making a complete cardiac evaluation obligatory when they persist during exercise or hyperventilation. In a study with 26 athletes and negative T-waves in the baseline ECG (marked repolarisation abnormalities), 4 had hypertrophic cardiomyopathy confirmed by echocardiography. The rest of them, in spite of their “pseudoischemic” ECG, had a tendency to normalise these alterations during exercise and had no clinical or pathological implications during follow-up [15]. Similar results were obtained in an another study with more than 1000 athletes, 5% of whom presented particularly abnormal ECG patterns with no evidence of structural heart disease [16]. In this study, patients were classified into 3 categories according to their ECG (normal or with minor alterations, mildly abnormal or distinctly abnormal). Although those with abnormal ECG presented larger cardiac dimensions as compared to those with normal ECG, none of them had abnormal values of wall thickness or diastolic volumes in the echocardiography [16].
The ECG of highly trained athletes can also show U waves from V2 to V4, usually associated to sinus bradycardia. Less frequently, a slight long QT is present, usually related to hydroelectrolyte alterations. Regarding QT interval, some recent reports establish that highly trained athletes with some degree of left ventricular hypertrophy do not present an increase of QT dispersion, in contrast to those with hypertensive cardiopathy. Thus, QT dispersion could be useful in distinguishing physiological from pathological hypertrophy [17;18].
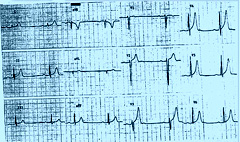
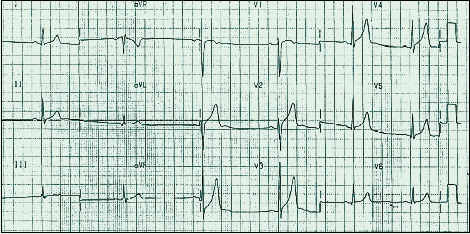
1- Vagotonic findings in an endurance sport practionner.
Vagotonic findings can be observed: sinus bradycardia, first degree AV block and typical vagotonic T waves.
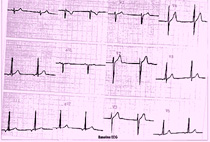
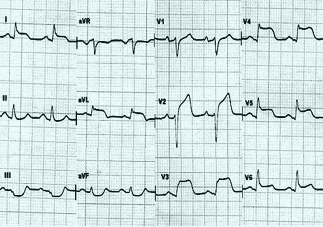
2- An ectopic atrial rhythm is observed in baseline ECG
2A) Baseline
Baseline rhythm in an 17-year-old athlete.

2B) During stress test
During the stress test, sinus rhythm appears with normal tachycardisation in an 17-year-old athlete.
Modified from Tntoré, S. Cardiología deportiva [3].
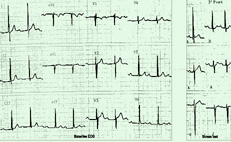
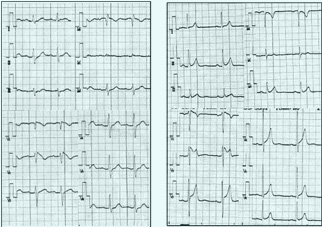
3) Baseline AV conduction disturbances that disappear during stress test.
3A) First degree AV block
3B) Second degree AV block
that disappear during stress test.
Modified from Tntoré, S. Cardiología deportiva [3].
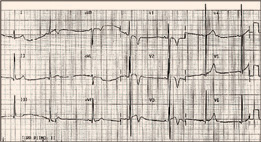
4) Different conditions that present ST-segment elevation in the ECG
4A) Early repolarisation :
Two examples of early repolarisation: elevation of J-point followed by high symetric narrow T waves (vagotonic T waves);
4B) Anterior acute myocardial infarction : ST-segment elevation with downward concavity, involving the end of the QRS complex and the T-wave;
 4C) Brugada syndrome
4C) Brugada syndrome
type 1: elevation of J-point with descendent ST-segment elevation and negative T waves (coved-type);
type 2: elevation of J-point with saddle-back ST- segment followed by negative or biphasic T waves.
5) Marked changes in repolarisation in a marathon-runner.
Marked repolarisation abnormalities are observed: asymmetric negative T waves from V1 to V3. The echocardiography did not show any structural disease.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.



 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.