ABBREVIATIONS
ACM: arrhythmogenic cardiomyopathy
ARVC: arrhythmogenic right ventricular cardiomyopathy
DCM: dilated cardiomyopathy
EF: ejection fraction
HCM: hypertrophic cardiomyopathy
HF: heart failure
HFmrEF: HF with moderately reduced EF
HFpEF: HF with preserved EF
HFrEF: HF with reduced EF
LV: left ventricular
RCM: restrictive cardiomyopathy
RV: right ventricular
Keywords: Cardiomyopathies, HFpEF, HFrEF, genetics, phenocopies
TAKE-HOME MESSAGES
- ESC HF guidelines indicate the need to identify the causes of HF because specific causes may correspond to disease-specific treatments
- Although HF is one of the most common manifestations of cardiomyopathies, the HF classification should be aligned in both cardiomyopathy subtypes and their evolutionary phases.
- Most cardiomyopathies and their phenocopies are heritable and transmissible genetic diseases; the precise diagnosis is mandatory especially when the cause affects treatments.
- Family segregation studies and deep phenotyping contribute to the interpretation of the numerous non-clinically actionable variants of unknown significance that limit the benefits of genetic diagnostics
Introduction
In the latest European Society of Cardiologists (ESC) Guidelines, heart failure (HF) is defined as "a clinical syndrome consisting of cardinal symptoms (e.g., breathlessness, ankle swelling and fatigue) that may be accompanied by signs (e.g., elevated jugular venous pressure, pulmonary crackles and peripheral oedema). It is due to a structural and/or functional abnormality of the heart that results in elevated intracardiac pressures and/or inadequate cardiac output at rest and/or during exercise". The guidelines distinguish between HF with preserved ejection fraction (EF) (HFpEF) and HF with reduced EF (HFrEF), and they introduce the concept of mildly reduced EF (HFmrEF), defined by a left ventricular EF ranging between 41-49%. The guidelines also specify that “the identification of aetiology is mandatory in the diagnosis of the HF because the precise cause can determine the treatments” and introduce the notion that “signs may not be present in the early stages of HF (especially in HFpEF) and in optimally treated patients” [1]. Compliance with both of these conditions (early diagnosis and determination of aetiology) requires diagnostic fidelity, in particular for cardiomyopathies with genetic origin, which goes beyond an EF-centred classification of HF. This text highlights the nosology of HF in cardiomyopathies, including genetic and acquired phenocopies, as well as the genetic workup required in daily clinical practice.
Heritable cardiomyopathies: a shared genetic path
"Cardiomyopathies are myocardial disorders in which the heart muscle is structurally and functionally abnormal, in the absence of coronary artery disease, hypertension, valvular disease and congenital heart disease sufficient to cause the observed myocardial abnormality" [2]. The ESC classification distinguishes hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), and restrictive cardiomyopathy (RCM) (Figure 1). Each cardiomyopathy is then grouped into genetic/familial and non-genetic/non-familial subtypes. In daily practice, the suspicion for familial cardiomyopathy stems from the clinical history of the family, the type of cardiomyopathy and associated cardiac and non-cardiac traits [3,4].
Figure 1. The figure shows the current classification frame of cardiomyopathy. The symbol flanking the different subgroups of cardiomyopathies indicates potential genetic diseases and aims to bring cardiologists back to the concept that medical genetics is always a family matter and not just a genetic test. A negative genetic test does not exclude a diagnosis of familial cardiomyopathies, when this is proven by clinical evidence.
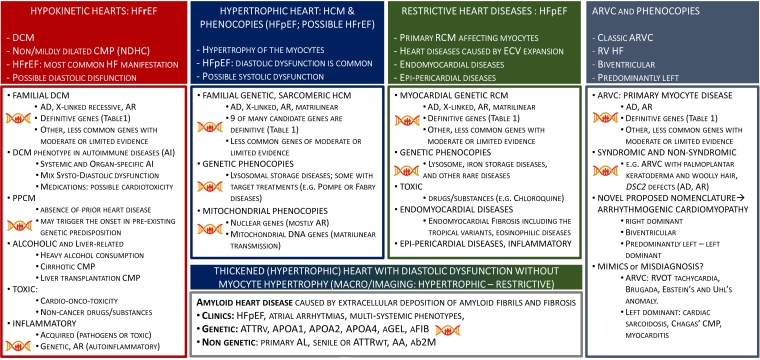
ARVC: arrhythmogenic right ventricular cardiomyopathy; CMP: cardiomyopathy; DCM: dilated cardiomyopathy; ECV: extracellular volume; EF: ejection fraction; HCM: hypertrophic cardiomyopathy; HF: heart failure; HFpEF: HF with preserved EF; HFrEF: HF with reduced EF; RCM: restrictive cardiomyopathy
Ideally, cardiologists suspecting familial cardiomyopathy first characterise the patient’s phenotype and then follow a path that includes genetic counselling and testing, and clinical family screening. When a pathogenic variant is identified in a cardiomyopathy-gene, cascade genetic screening of relatives is undertaken [4]. Although many disease genes have been proposed in the last 20 years, relatively few are classified as “definitive” (Table 1). This does not diminish the importance of genes with moderate or limited evidence of association with cardiomyopathy, but rather calls for the implementation of careful analysis of phenotypes and their segregation with genotypes. In this regard, cardiologists have an essential role [5] in the validation of the pathogenicity criteria, especially for variants of uncertain significance [6]. Importantly, apparently sporadic phenotypes do not exclude a genetic cause that can be a de novo genetic defect [5] and, in turn, can be transmitted to the progeny.
Table 1. The table summarises the cardiomyopathy genes and related phenotypes as curated by authoritative experts. The two highlighted genes, LMNA (violet) and MYBPC3 (green),
are examples of genes that have been associated with different cardiomyopathies, but their definitive association typically remains in the original phenotypical context of identification (DCM for LMNA and HCM for MYBPC3). Similar observations apply to many other genes.
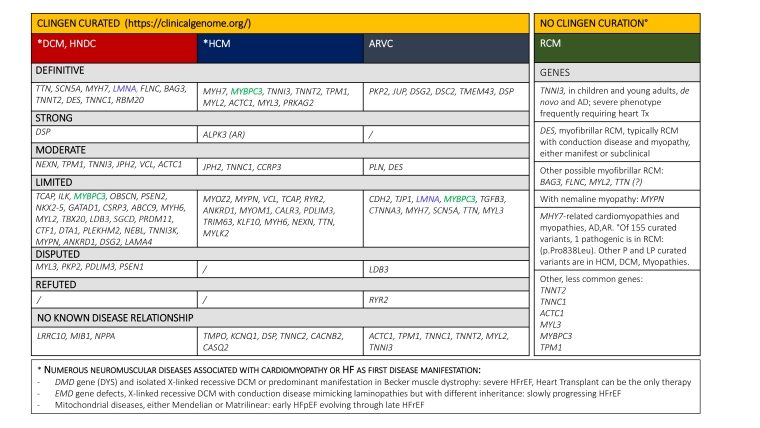
AD: autosomal dominant; ARVC: arrhythmogenic right ventricular cardiomyopathy; DCM: dilated cardiomyopathy; EF: ejection fraction; HCM: hypertrophic cardiomyopathy; HF: heart failure; HFpEF: HF with preserved EF; HFrEF: HF with reduced EF; HNDC: hypokinetic non-dilated cardiomyopathy; RCM: restrictive cardiomyopathy; Tx: transplant
HF is one of the main clinical manifestations of all cardiomyopathies. DCM paradigmatically manifests with HFrEF, RCM with HFpEF. HCMs can show either diastolic dysfunction with preserved or enhanced systolic function, or, less commonly, systolic dysfunction. HF may also occur in ARVC with preserved left ventricular (LV) function. However, the type of cardiomyopathy may not precisely coincide with the HF classification because both systolic and diastolic dysfunction can co-exist in patients with cardiomyopathy; this carries a clinical significance that influences treatment and prognosis. Therefore, beyond the paradigmatic HFrEF in DCM and HFpEF in RCM, the classification of HF in cardiomyopathies should also be framed in the context of their different phases of development.
DCM and DCM-like phenotypes
DCM is characterised by LV dilatation and LV systolic dysfunction in the absence of other disorders sufficient to cause global systolic impairment. RV dilatation and dysfunction may be present but are not necessary for the diagnosis [2] (ESC, 2008: familial and non-familial forms are acknowledged). The "hypokinetic non-dilated cardiomyopathy" is a recently classified entity that incorporates the diagnostic criteria in probands as well as in relatives, also integrating the possible genetic cause [7]. In this context, the concept of "early diagnosis" is particularly useful to describe the phenotypes observed in family members who do not yet fulfil the diagnostic criteria for DCM.
The search for a precise aetiology should primarily address the distinction between monogenic DCM vs similar phenotypes that can be observed in inflammatory, autoimmune and toxic myocardial conditions. Cardiologists are aware that DCM may have genetic bases and are attentive to the family data, as well as to cardiac and extracardiac traits (e.g., red flags) that can contribute to suspect genetic DCMs [3,4].
In familial genetic DCM, it is clinically useful to assess the mode of transmission, the presence of cardiac (e.g., atrioventricular [AV] block) or extracardiac (e.g., neuromuscular involvement), or systemic manifestations (e.g., syndromic DCM) [3,4,8,9].
In inflammatory DCM, often following infectious myocarditis, the diagnosis is based on chronic myocardial inflammation and fibrosis, associated with persistent LV dysfunction and ventricular remodelling [10], and thus requires the demonstration of myocardial inflammation.
With a few exceptions of rare genetic autoinflammatory diseases (e.g., Familial Mediterranean Fever, tumour necrosis factor receptor-associated periodic syndrome [TRAPS], etc.), these diseases are usually acquired.
In peripartum cardiomyopathy (PPCM), defined as "rare life-threatening cardiomyopathy of unknown cause that occurs in the peripartum period in previously healthy women", the diagnosis is made when the phenotype manifests in the narrow peripartum time window and requires echocardiographic evidence of LV systolic dysfunction. By definition, the diagnosis relies on absence of cardiac dysfunction before pregnancy, but this is rarely documented. PPCM is potentially reversible but, importantly, PPCM can unmask pre-existing genetic DCM or manifest in genetically predisposed women [11].
A DCM phenotype may follow the administration of different classes of chemotherapeutic agents for cancer: e.g., Anti-Her2, Fluoropyrimidines, Tyrosine kinase inhibitors, proteasome inhibitors; immunotherapies: immune checkpoint inhibitors and Chimeric Antigen Receptor T-Cell (CAR-T) therapy [12]. When patients with cardiomyopathy (genetic and non-genetic) develop cancer, individual monitoring plans of the LV function and rhythm disturbances should be considered to best manage both conditions.
Non-cancer drug cardiotoxicity affecting systolic function can occur in patients with a previously healthy cardiovascular system, as well as in patients with pre-existing cardiovascular diseases; when recognised, this is potentially reversible with the removal of the toxic cause.
In "alcoholic cardiomyopathy", the cause is chronic heavy alcohol consumption; however, TTN gene mutation carriers are particularly predisposed to the risk of alcoholic cardiomyopathy [13]. Potentially related to alcoholic cardiomyopathy are cirrhotic cardiomyopathy, which is characterised by chronic cardiac dysfunction with impaired contractile responsiveness to stress and/or altered diastolic relaxation [14], and liver transplantation-related cardiomyopathy [15].
Finally, although heart involvement is not a diagnostic criterion for any autoimmune diseases -either systemic or organ-specific - the heart is commonly involved.
The hypertrophic heart: myocyte thickening vs extracellular volume expansion
Disease of cardiomyocytes
"HCM is defined by the presence of increased left ventricular (LV) wall thickness that is not solely explained by abnormal loading conditions [16]” (estimated prevalence ranging between 0.02 and 0.23% in adults). Clinical manifestations include arrhythmias, HF, and thromboembolic complications. HCM is the most common cardiac genetic disease. The genetic causes are heterogeneous, but the clinical diagnostic path is well described and supported by risk stratification tools [17]. Genetic testing is recommended (Class I, Level B) when the disease cannot be explained solely by a non-genetic cause, whether or not clinical or genetic testing will be used to screen family members. In primary HCM, the increased myocyte size depends on the amount, organisation and metabolism of sarcomeric components. At present, the disease gene and mutation do not condition the prescription of specific therapies [18].
Genetic phenocopies of HCM include diseases in which the myocyte thickness reflects intracellular accumulated material (for example, lysosomal storage disorders). The precise diagnosis is mandatory because target therapies are available for many of these diseases. In mitochondrial cardiomyopathies, the thickened LV is usually symmetrical and the HCM is non-obstructive. HF, when present, is with preserved EF, while end-stage cardiomyopathy is characterised by HFrEF. The disease is either maternally inherited, when associated with mutations in mtDNA genes, or Mendelian (mostly autosomal recessive), when caused by defects in nuclear genes encoding mitochondrial proteins/subunits. In iron overload diseases, the increased myocyte size depends on the intra-myocyte iron accumulation. The genetic causes are heterogeneous, with HFE as the most common form in Europe; other less common genes are HJV, SLC40A1, TFR2, FHT1, HAMP, and BMP2. A peculiar iron storage disease is the mitochondrial iron overload in Friedreich ataxia that is transmitted as an autosomal recessive trait and is characterised by severe loss of expression of frataxin.
Differential diagnoses include non-genetic heart diseases with myocyte hypertrophy and non-substitutive fibrosis, such as hypertensive heart disease, aortic valve diseases and aortic coarctation or hyperkinetic conditions, that potentially reverse with removal of the cause. In athletes, the myocyte thickness depends on the increased intracellular amount of the sarcomeric components; the thickness may decrease with detraining. Criteria for differential diagnosis between HCM and athlete’s heart are well established and genetic tests should not be improperly performed.
Expansion of the extracellular space
Increases in myocardial wall thickness can be caused by expansion of the extracellular space. The archetype is cardiac amyloidosis, which is characterised by the deposition of amyloid fibrils in the interstitial space, valves, vessels and epi-pericardium. The myocardial thickening results from the burden of extracellular deposition of amyloid fibrils that is often accompanied by fibrosis. Myocytes are the bystanders of the fibril deposition but may also suffer direct toxicity in amyloid light chain (AL) amyloidosis. Although amyloidosis is included in the group of HCM, there is no hypertrophy of the myocytes; vice versa, the diameter of the myocytes decreases with the increase of amyloid deposition. Furthermore, the typical diastolic dysfunction induces to place cardiac amyloidosis in the RCM group, despite the wall thickness being severely increased, exceeding normal or nearly normal values that contribute to the definition of primary RCM. HF is the main determinant of prognosis; the onset can be subtle and the precise diagnosis suffers as a result of consistent diagnostic delay. EF is typically preserved but can decrease, especially when the involvement of small intramural vessels adds multifocal, non-adjacent ischaemic damage. The identification of the precise cause of amyloidosis is an obligate diagnostic step because it determines the administration of target treatments [19].
Restrictive physiology and restrictive cardiomyopathy
A restrictive ventricular filling pattern occurs when increased myocardial stiffness causes ventricular pressure to rise precipitously with only a small increase in volume. It can be observed in restrictive, hypertrophic and dilated cardiomyopathies; endomyocardial diseases; epi-pericardial diseases; as well as in cardiac diseases other than cardiomyopathies. In this context, the restrictive cardiomyopathy is defined by restrictive ventricular physiology in the presence of normal or reduced diastolic volumes of one or both ventricles, normal or reduced systolic volumes and normal ventricular wall thickness [2]. Atrial enlargement is a common feature of the disease.
Restrictive myocardial diseases can be grouped as primary genetic (e.g., TNNI3 gene defects [20] or restrictive cardio-myofibrillar diseases, such as desminopathies [21]) (Table 1), genetic phenocopies that may partly overlap with HCM (e.g., lysosomal or iron storage diseases), and acquired phenocopies (e.g., hydroxychloroquine drug toxicity). Genetic testing should be performed in both primary RCM and genetic phenocopies, while toxic causes should be recognised and removed to restore myocardial function.
Acquired endomyocardial diseases functionally mimicking RCM include endomyocardial fibrosis (EMF) associated with hypereosinophilic syndromes. These latter require somatic genetic testing to identify fusion genes (e.g., FIP1L1-PDGFRA) that cause hypereosinophilic clonal expansion highly responsive to specific treatments (e.g. imatinib).
Phenocopies include Hedinger syndrome or carcinoid heart syndrome in patients with neuroendocrine tumours. Most epi-peri-cardial diseases affecting diastolic function represent the fibrotic evolution of inflammatory pericarditis with acquired causes, with the rare exceptions of genetic autoinflammatory diseases [10].
Arrhythmogenic right ventricular cardiomyopathy
HF is a less common manifestation in ARVC which is “defined histologically by the presence of progressive replacement of RV myocardium with adipose and fibrous tissue often confined to a 'triangle of dysplasia' comprising the RV inflow, outflow, and apex” [22]. The disease is typically caused by defects in genes coding desmosome proteins. The 2010 Task Force formulated the criteria for definite, borderline or possible diagnosis, through combinations of major and minor criteria in 6 clinical categories: 1) global or regional RV dysfunction (LV function and size can be normal); 2) structural abnormalities (fibro-fatty replacement of myocytes); 3) anomalies of repolarisation; 4) anomalies of depolarisation; 5) arrhythmias; and 6) familial history and/or presence of pathogenic genetic variants.
The inappropriate use of the TF2010 criteria led, 10 years later, to a critical revision of these criteria and to the proposal of new solutions capable of improving the characterisation of the left- sided and paediatric forms. The new proposed classification includes, in addition to the classic right-dominant form, the biventricular and left-dominant variants, unified under the term “arrhythmogenic cardiomyopathy" (ACM) [23]. This term, however, can encompass all cardiomyopathies, since for different causes and pathologic substrates, all cardiomyopathies are potentially arrhythmogenic. In ARVC, the main clinical attention is focused on the risk of life-threatening arrhythmias and prevention of sudden cardiac death. ARVC less commonly causes HF, although the recent proposal to distinguish classic (right), biventricular and mainly left ARVC complicates the nosology classification and often makes it difficult to avoid overlapping and misdiagnosis.
Right ventricular ejection fraction, however, can be severely impaired and complicated by pulmonary thromboembolic events, with heart transplantation required even in patients with normal LV size and function. The list of clinical mimics includes both genetic (Table 1) and non-genetic diseases such as myocarditis and sarcoidosis, both potentially treatable but distinct diseases.





 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.