Introduction
Is it possible to write a historical paper on the aortic valve? To modern cardiologists, the aortic valve has always been a fact, with a large range of diagnostic and therapeutic options at our disposition. But how and when was this knowledge built? Who developed the technologies? Standing on the shoulders of our predecessors, we should not take our current knowledge for granted. Insight into how we have come this far will increase our appreciation of all the possibilities we have to treat our patients.
Early History of Anatomy and Physiology
The foundations for anatomy and embryology in the Western world were laid by Aristotle (384 BCE-322 BCE), a pupil of Plato in Athens. By studying the entire world of living things, he is regarded as being the first great biologist [1]. Greek culture shifted to Alexandria, where a famous medical school was established about 300 BCE. Its two best medical teachers were Herophilus, whose manuscripts on anatomy may have been the first of their kind, and Erasistratus, regarded as the founder of physiology. Erasistratus thought that nerves were hollow tubes containing fluid, and that air entered the lungs and heart and was carried through the body in arteries [1].
During the early centuries of the Christian era, many Greek doctors moved to Rome. The most famous of them was Galen of Pergamum or Claudius Galenus (129 CE-216 CE) [2]. Galen regarded anatomy as the foundation of medical knowledge and dissected a range of animals, mostly monkeys. He was among the first to describe the valves of the heart. He also saw the structural differences between arteries and veins. One of his most important demonstrations was that arteries carry blood, not air, as had been taught for 400 years [1]. However, circulation was still not understood. Galen believed that nutrients and venous blood went partly through pores in the intraventricular septum, and in the meantime came into contact with pneuma, leading to formation of arterial blood [2].
The first accurate drawing of the aortic valve was by Leonardo da Vinci in 1512 (Figure 1). Anatomist Andreas Vesalius (1514-1564), born in Brussels (Belgium), changed Galenic thinking [2]. After Louvain and Paris, he went to Padua (Italy), one of the most prominent universities after Bologna in the Renaissance period [2]. By performing autopsies on humans instead of animals, he discovered Galen’s mistakes. He wrote his key work in 1543, “De Humani Corporis Fabrica” [2-4]. This is regarded as the largest single contribution to medical science [2]. He became so famous after this publication that he immediately became the doctor of Emperor Charles V, as well as of his successor Philip II [2]. However, the concept of circulation had still not been revealed. Building on Vesalius’ work, William Harvey (1578-1657) discovered the property of veins, publishing his findings in his key manuscript “De motu cordis” (1628) [3]. He concluded that blood circulates in a single direction, with the heart as a mechanical pump (5).
Figure 1. Leonardo Da Vinci (Vinci 1452-Amboise 1519)
The Aortic Valve c.1512-13.
Pen and ink on blue paper | 28.3 x 20.4 cm
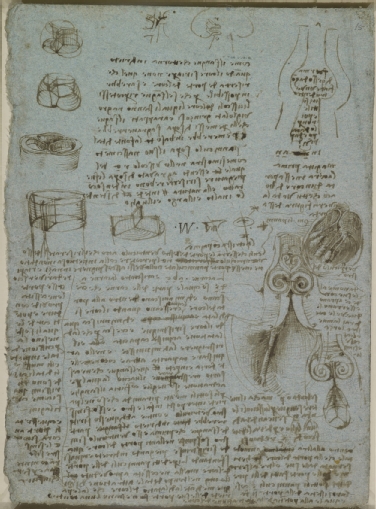
Royal Collection Trust / © Her Majesty Queen Elizabeth II 2019
Medical Technology
The Stethoscope
In the early 1800s, a young French physician was called to examine a young woman. At that time, René Laënnec (1781-1826) was chief physician to the Hôpital Necker in Paris and had been studying with Jean-Nicolas Corvisart (1755-1821), personal physician to Napoleon [1]. In those days, social relationships and rules were very strict, and Laënnec was not permitted to lay his ear on the chest of the female patient, so he had to invent something. He developed a simple wooden cylinder about 23 cm (9 inches) long that could be unscrewed for transport. The stethoscope was “born” (Figure 2) [5,6]. Laënnec published his results in his classic treatise “De l’Auscultation Médiate” in 1819 [7]. The first stethoscope was monaural. American born, but with German parents, George Cammann (1804-1863) claimed the invention of adding two earpieces, thus making it binaural in 1852 [5]. But it was the Irish physician and world traveller Arthur Leared (1822-1879) who had already exhibited “a double instrument with gutta percha tubes” at The Great Exhibition in London in 1851 [8].
In 1831, the British physician James Hope was the first to classify murmurs in “A Treatise on the Disease of the Heart and the Great Vessels” [6,9].
Figure 2. Lithograph “Laennec a L’Opital Necker Auscultate un Physique” (1816) from a painting by Chartran, classical French painter (1849-1907). Under the image “D’Apres T Chartran” is engraved on the left, “Heliogravure” on the right.
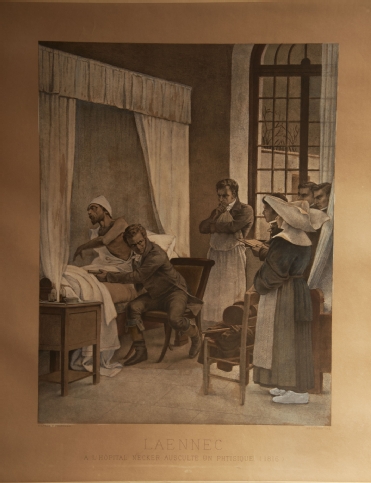
Courtesy of M. Donald Blaufox, MD, PhD
https://www.mohma.org/instruments/category/stethoscope/laennec_lithograph/
Blood Pressure Measurement
French physicist and physiologist Jean Poiseuille (1797-1869, who gave his name to Poiseuille’s law) was very interested in the flow of blood in vessels. In 1828 he presented a mercury manometer device to measure blood pressure [6]. It was the Italian Scipione Riva-Rocci (1863-1937) (hence the denomination RR for blood pressure) who in 1896 introduced the inflatable arm cuff which was coupled to a sphygmograph [6]. Nicolai Korotkoff (1874-1920), a Russian military surgeon, was the first to auscultate the brachial artery sounds in 1905 [6].
X-ray
Another spectacular advance in diagnostic possibilities was the discovery of X-rays in 1895 by the German Wilhelm Conrad Röntgen (1845-1923) [1,5]. In 1908 another German, Morris Simmonds (1855-1925), used X-rays to show valvular calcifications after death for the first time [10]. The American Merrill Sosman (1890-1959), amongst others, diagnosed aortic stenosis (AS) in 1924 in Boston using X-rays in a living person [10].
Catheterisation
The first attempt to enter the heart with a catheter, albeit in a horse, was performed by Frenchman Claude Bernard (1813-1878) in 1844. He managed to reach the left and right ventricles using a catheter via the jugular vein and carotid artery [11]. In 1929, the German Werner Forssmann (1904-1979), at that time working in Eberswalde, had another idea and used himself as a guinea pig; he passed a catheter in his left arm up until the right atrium, using fluoroscopy via a mirror held by a nurse. He then took the stairs to the radiology department to document this on a chest X-ray. Later he decided to become a urologist [6,11].
However, it took until 1950 for the first retrograde left catheterisation to be performed by the American Henry Zimmerman (1915-2007) in Cleveland, as well as Limon Lason in Mexico [11]. Zimmerman was the first to measure left ventricular pressure in 10 patients with aortic regurgitation (AR) [12]. In 1950, the Cuban Rodrigo Bustamente Marcayda was the first to observe AR after injecting contrast in the aorta [12]. In 1953, Swede Sven Ivar Seldinger (1921-1998) developed the percutaneous technique. In 1959, the American F. Mason Sones (1918-1985) was trying to inject contrast dye into the aorta of a young man, but his catheter tipped into the right coronary artery (RCA). Before he could ask to pull back the catheter, a large dose of contrast was already injected, and the RCA was depicted. The patient immediately had an asystole but after coughing his heart rhythm was restored. By serendipity he had just completed the first selective coronary angiography in Cleveland [6,11].
In 1956, Cournand, Forssmann and Richards received the Nobel Prize for their work on heart catheterisation [5].
Echocardiography
The importance of echo reflection was first demonstrated by the Italian Lazzaro Spallanzani (1729-1799). He demonstrated that bats use reflected echoes of inaudible sounds to fly and navigate [13]. Only after the discovery of piezoelectricity in 1880 by Pierre Curie and his brother Jacques did it become possible to create ultrasonic waves [13]. Major advances were bolstered by two wars. Frenchman Paul Langevin (1872-1946) developed Sound Navigation and Ranging (SONAR) in 1915 to detect enemy submarines, followed by the US navy using Radio Detection and Ranging (RADAR) in 1941 to detect planes. Ultrasonic pulse-echo was first used by the Soviet Sergei Sokolov in 1937 to detect flaws in metals [13].
It took several decades before this technology was used in cardiology. The founding father is the Swede Inge Edler (1911-2001). During the late 1940s, Edler, as head of the Cardiovascular Laboratory in Lund, was responsible for preoperative evaluation of (mitral) valve disease for his pioneering heart surgery colleagues Wulff and Sandblom [13]. However, Edler was not happy with his cardiac catheterisation results. He had read a book on RADAR and wondered whether this could be the solution for non-invasive use. Via Jan Cederlund, he came into contact with Carl Hellmut Hertz, son of Nobel Prize Physics winner Gustav Hertz, and nephew of Heinrich Hertz (who gave his name to the unit of frequency). They were lent the first ultrasonic reflectoscope from a shipyard to do some experiments during the weekend. To their fascination, they saw an echo moving back and forth on the oscilloscope screen at a depth of 8-9 cm from the chest wall. Without funding, luckily, they found out that Siemens was building an ultrasonic reflectoscope. Siemens’ boss Gellinek sent the scope to Lund to use for one year; it never went back. After testing and experimenting, they chose 2.5 MHz as the optimal frequency [13]. On 29 October 1953, equipped with the Ultraschall-Impulsgerät, Edler and Hertz recorded the first moving pictures of the heart, thus inaugurating the field of “ultrasound cardiography” [13].
Edler and Hertz also attempted transoesophageal echocardiography (TEE) but encountered several difficulties. The credits for the first TEE (performed in Chicago) go to American Leon Frazin in 1976 [13,14]. Two-dimensional echocardiography was introduced in 1974 [6], pulsed Doppler haemodynamics in 1975, and Doppler colour flow in 1982 [6]. Transoesophageal imaging in 1985 made a large contribution to very specific images of cardiac valves [6].
In the USA, Harvey Feigenbaum gave the first course on cardiac ultrasonography in 1968. Feigenbaum is said to have introduced the term “echocardiography” [13].
Aortic Regurgitation (AR)
Galen and Da Vinci understood that the function of the aortic valve was to prevent a reversal of flow [12]. Early descriptions of AR were made in 1706 by London surgeon William Cowper (1666-1709), who also found an enlarged heart on autopsy - “larger than an ox”, hence the name cor bovinum [6,12]. In 1715, French physician Raymond Vieussens (1641-1716) described the collapsing pulse in AR and also confirmed on autopsy an enlarged left ventricle besides the “markedly stretched valves” [6,12]. In Padua in 1761, Italian Giovanni Battista Morgagni (1682-1771) recognised the important haemodynamic consequences of AR [6,12].
In 1832, Englishman James Hope (1801-1841) described a prolonged murmur after the second heart sound [2]. In the same year, Dublin surgeon Sir Dominic Corrigan (1802-1880) provided the classic description of the arterial pulse and also the murmur of AR [6,12]. He noted two other signs - a “bruit de soufflet” over the ascending aorta, carotid and subclavian arteries, as well as a “frémissement” (thrill) over the carotid and subclavian arteries [12]. It was Thomas Watson who, in 1843, linked this pulse, also called pulsus celer, to a water hammer ([2,15]. A water hammer was a Victorian toy in which a tube was half filled with fluid, the remainder being a vacuum. Each time the tube was inverted or shaken, the impact of the fluid at each end would sound like a hammer blow.
In the mid-19th century, Americans who had studied in Paris tried to popularise the use of the stethoscope in the USA. The “American Laënnec” was Austin Flint (1812-1886) [16].
In 1862, he described two patients with AR, each of whom had a diastolic murmur similar to the one heard in mitral stenosis. Flint believed that such a murmur could be produced without any mitral lesions. The regurgitant stream of blood was thrust into the stream leaving the left atrium, thereby setting the mitral leaflets into vibration, which was responsible for the murmur [12,15].
In 1861, Frenchman Paul Louis Duroziez (1826-1897) described an intermittent double murmur over the femoral artery as a sign of AR (“Duroziez’s sign”). The first murmur, resulting from the powerful contraction of the left ventricle, was perceived by pressing the femoral artery 2 cm above the stethoscope; the second murmur (diastolic), believed to be the result of contraction of the arteries in the legs, was heard by pressing the femoral artery 2 cm below the stethoscope [12]. This is not the same as Traube’s sign (Ludwig Traube, 1818-1876, German physician), which is a double tone heard without compressing the femoral artery. The systolic sound, likened to that of a pistol shot, may be due to the sudden distention of the arterial wall [12]. The synchronous nodding of the head with the heart beat was observed in 1900 by Frenchman Delpeuch, who named it “de Musset’s sign” (after a French poet with AR) [12].
Aortic Stenosis (AS)
AS was first described in 1663 in “Opera Medica Universa” by Frenchman Lazare Riviere (1589-1655), based on a patient seen in 1646 [10]. It was also described by the founder of pathological anatomy, Giovanni Battista Morgagni [4,10]. Jean Nicolas Corvisart mentioned an aortic valve “ossified and united so closely that the end of a little finger could scarcely be introduced” [10]. In 1819, Rene Laënnec pointed out that the aortic valve was subject to ossification [6,10].
In the first half of the 20th century, investigators debated on the different causes of AS [10]. A congenital cause of AS was largely ignored; however, the bicuspid aortic valve had already been described in 1844 by British surgeon Sir James Paget (1814-1899) [10].
James Hope provided details of AS auscultation in 1832 [6,10]. Irishman William Stokes (1804-1878) wrote a case on a man who dropped dead from extreme AS [10]. In 1955, Reinhold recorded with phonocardiography a loud early ejection click in a patient with a congenital AS [10].
Besides X-rays, catheterisation was also used, in the beginning via needle punctures. It took years before gradients and left-sided pressures were measured via retrograde arterial catheterisation [10]. In 1950, Limon Lason reported measurements of left ventricular and aortic pressure in AS patients, using a radial artery approach [10].
In 1933, grading of systolic murmurs was introduced in Boston by the Polish born (but living in America from the age of 3) Samuel Levine (1891-1966) [6]. The acoustic principles of cardiovascular sound improved considerably thanks to the work of Rappaport and Sprague in the 1940s [6].
Aetiology
The aetiology of valvular disease in the 19th and first half of the 20th century was mainly about highly prevalent rheumatic fever and gonorrhoea [6]. Infections, such as streptococcal ones, could not be treated as antibiotics had not yet been invented. Doctors only had their stethoscope to examine patients. Improved diagnostic technology yielded other causes of valvular disease. After degenerative calcification, from 1997 the central hypothesis of AS was inflammation of the aortic valve in patients with atherosclerotic risk factors [6,17]. Currently, hallmark features are early atherosclerosis, cell proliferation and osteoblast expression [17].
Valve Surgery and Interventions
In 1913, Frenchman Theodore Tuffier (1857-1929) performed the first operation for AS at the Hôpital de la Pitié in Paris, France. He wanted to incise the stenosed valve but eventually performed a digital dilatation [10]. In the 1920s most interventions were performed on the mitral valve. In 1950, in the Mayo Clinic, American Robert Glover used a dilating instrument on the aortic valve commissurotomy instead of a finger for AS [10].
The next important development in the surgical management of aortic valve disease was the successful implantation of an acrylic ball valve prosthesis in the descending thoracic aorta in a 30-year-old woman with severe AR. This was carried out by Charles Hufnagel in 1952 in Washington DC [10,12,18]. In 1956, Irishman Jeremy Swan (1922-2005, co-inventor of the Swan-Ganz catheter) and Kortz performed the first direct vision commissurotomy for AS, using an ice bath for hypothermia at the Mayo Clinic, Rochester, MN, USA [10].
After the heart-lung machine was designed, Boston surgeon Dwight Harken (1910-1993) was, in 1960, able to implant the first prosthetic valve in the aortic position for AR [12,19].
Walton Lillehei (1918-1999) is regarded as the father of open-heart surgery. He was born in Minneapolis to a Norwegian family [20]. In 1957 he performed the first intracardiac aortic valve replacement with a plastic prosthesis [20]. He was involved in the development of several types of valve, such as the St. Jude valve [20]. During his cardiac surgeries, Lillehei had noted that quite often patients showed conduction disturbances. He was the first to implant an internal cardiac pacemaker, which was at that time connected to an external power source. This gave rise to a lot of practical problems. He called on his electrical engineer Earl Bakken to think of a solution. The rest is history: Medtronic was founded in a garage in Minneapolis in 1958 [20].
In 1960, in Boston, Harken replaced a stenosed aortic valve below the level of the coronary ostia with a caged-ball prosthesis [10,18]. This was at a time when there was great enthusiasm for this type of prosthesis, after an initial report by Albert Starr (physician) and Lowell Edwards (electrical engineer) [18]. This caged-ball type was initially designed for the mitral valve [18].
The first catheter-based approach to balloon aortic valvuloplasty (BAV) was developed by Frenchman Alain Cribier in 1985 [21]. It was the Dane, Henning Rud Andersen who, in 1988, speculated that, just like a coronary stent, a balloon-expandable valve could be placed, namely transcatheter aortic valve replacement (TAVR) [21]. He could not find a company to develop this, but Cribier with others formed a start-up company. In 2002, he took the credit for the first human percutaneous transcatheter aortic valve implantation (TAVI), performed in Rouen, France [21]. Later, the life of Henning Rud Andersen’s father was saved by the invention of his son, as he regained his life after a TAVI procedure.
Conclusion
Although it is impossible to mention everybody who played a role in the discovery, developments and inventions regarding the aortic valve, this paper provides some insight into the great names involved. Europe played an important role in the development and invention of diagnostic instruments in the early days and since, due to worldwide collaborations, the medical field has progressed. This historical knowledge can inspire us to think beyond imagination, as our predecessors did.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.