Background
Bicuspid aortic valve (BAV) is the most common congenital cardiac abnormality, affecting approximately 1%-2% of the general population. (1,2) Adverse cardiac outcomes related to the valve and/or root (3) put a large burden on cardiovascular patients, in addition to the many undergoing aortic valve replacement who will also need aortic root surgery.
Although inheritance is variable, it is a familial disease (4,5) with an estimated 10% chance of a first degree relative being affected (6,7) and 20%-30% when aortopathy is included into the calculation. (8,9) Additionally, certain gene mutations (NOTCH1) have been associated.
The BAV is composed of not three aortic normal leaflets - as in the normal tricuspid valve - but two abnormal leaflets, usually unequal in size, possibly resulting from inadequate fibrillin-1 production during valvulogenesis. (10)
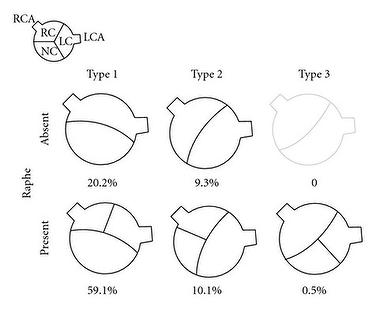
The most common form has the two commissures located in an anteroposterior direction giving left and right cusps. Less common is having the commissures located on the right and left sides of the annulus leading to anterior and posterior cusps. Type 1 BAVs are more likely to stenose as adults while type 2 valves will have complications earlier. Rarely, there is fusion of the left and non-coronary cusps. A raphe is present on the right and anterior cusps, respectively, and this can make the valve appear tricuspid on echocardiography (Figure 1). (11)
Figure 1: Classification and Incidence of BAV.
Complications
Complications are 1) aortic stenosis 2) aortic regurgitation (or incompetence) 3) endocarditis. Calcification usually also occurs.
Due to abnormal stresses, even a normally functioning BAV can progress and damage gradually to reveal abnormal folding and creasing throughout the cardiac cycle with more turbulent flow, as well as restricted motion. (12)
Aortopathy and coarctation have implications on the prognosis of BAV. In several cohort studies, the long-term survival of patients was similar to the normal population, but with more cardiac events and need for surgical interventions on the valve and/or aorta. (13,14) Natural history of BAV ranges from severe aortic stenosis in childhood to longstanding asymptomatic disease into the elderly years.
- Aortic stenosis is the most common complication and may require surgery, most often necessary in middle age. (15,16) Only 15% of patients with BAV will have a normal function in the fifth decade.
- Aortic regurgitation also occurs due to the abnormality and may present with or without aortic stenosis. (17) Various aetiologies have been suggested to explain the mechanism of aortic regurgitation in BAV, including cusp prolapse, endocarditis, dilated aortic root, and myxoid degeneration of the valve. (18)
- Endocarditis is more common in BAV than in the normal tricuspid aortic valve. The incidence is estimated to be less than 2% in different series, but the outcome of endocarditis tends to be worse than in normal valves.
Aortopathy
Aortopathy refers to 'dilated aortic root'. It is usually associated with BAV and may lead to aortic aneurysm, dissection and rupture. (19,20) The prevalence of ascending aorta dilatation in patients with BAV ranged from 7.5% to 79%, according to the study of aortas in the population and region examined. (21-22) Incidence was higher in patients with fusion of the right and non-coronary cusps than the more common phenotype of fusion of the right and left coronary cusps. The mechanism of aortopathy is explained by genetic theory (aortic root fragility and elastic fragmentation due to inherited developmental defect) and hemodynamic theory (abnormal stress on aortic root due to turbulent flow through BAV). (23-27)
Three different shapes of proximal aorta in BAV were described and co-related to the type of BAV cusp configuration. (28) Serial echocardiographic examinations found higher rates of growth at all levels of the proximal aorta above the annulus in patients with BAV in comparison to those with tricuspid aortic valves. (29-31) Aortic dissection is a lethal sequel in patients with BAV and occurs at a younger age. Recent data suggest that BAV increases the risk of aortic dissection nine-fold over that in the general population. (32).Its incidence is less than 1% more in some studies, yet reaches 4% in others. (33)
It is worth noting that aortic root dilatation is an important predictor of dissection and rupture in BAV-associated aneurysms, even if the aortic valve is functioning normally. (34)
Coarctation of aorta
Coarctation of aorta is another major abnormality that can be associated with 20% or more of BAV. In the presurgical era, this association was found to increase the risk of death from aortic dissection more than if coarctation existed without BAV. (35) Coarctation is sometimes regarded as a part of the diffuse aortopathy associated with BAV.
Less common congenital anomalies associated with BAV include ventricular septal defects, Ebstein’s anomaly, hypoplastic left heart syndrome, abnormal coronary anatomy, patent ductus arteriosus, atrial septal defects and bicuspid pulmonary valve.
Diagnosis
Echocardiography: The mainstay of diagnosis is echocardiography (transthoracic or transoesophageal) which can provide a definitive diagnosis in the majority of patients with 92% sensitivity and 96% specificity when images are adequate (36). The echocardiographic report should adequately evaluate aortic valve morphology and measure the severity of any stenosis or regurge. It should also include aortic measurements at the aortic annulus, sinuses, sinotubular junction, and mid-ascending aorta.
Doppler: In addition, evaluation for aortic coarctation using Doppler interrogation of the proximal descending aorta should be performed. Aortic magnetic resonance angiography or CT angiography is indicated if morphology of the aortic root and/or ascending aorta cannot be assessed accurately or fully by echocardiography.
As recommended by the recent north American and European guidelines, patients with BAV who have documented dilation of aorta should have serial assessment of aortic morphology to detect progression of aortopathy early enough before complications occur (37). Recent tools for diagnosis and risk stratification have been suggested using metalloproteinase plasma assays and magnetic resonance imaging (38).
Treatment
Aortic valve replacement is the only definitive treatment for BAV associated with severe stenosis and/or regurgitation. The indications for surgery are similar to those with tricuspid aortic valve.
New techniques of repair such as transcatheter aortic valve implantation have also been reported in BAV (39) but are still considered as a relative contraindication in recent guidelines. In patients who refuse surgery or are not candidates for surgical intervention, medical therapy is limited and is mainly used to treat existent cardiac conditions such as heart failure, coronary artery disease or hypertension.
However, there is a possible role of beta blockers and ARBs in delaying progression of aortic dilatation, extrapolating from patients with aortopathy associated with Marfan’s syndrome, but have not been confirmed in clinical studies.
Guidelines
The recent ESC guidelines for valvular heart disease management recommend that sugery should be considered for any patient with aortic root diameter of ≥55 mm (Table 1). However, in patients with BAV, surgery in aortic diameters of ≥50 mm should be based on patient age, body size, comorbidities, type of surgery, and the presence of additional risk factors - family history, systemic hypertension, coarctation of the aorta, or increase in aorticdiameter ≥2 mm/year in repeated examinations using the same technique and confirmed by another technique.
The new ACC/AHA guidelines recommend surgical repair of aortic root if aortic root diameter is ≥5.5 cm (Class I). This recommendation changed in 2014 from the previous 2006 recommendation which had a cutoff value of 5 cm.
It should also be noted that the ACC/AHA guidelines considered the evidence of rapid progression of a maximum aortic cross-section: body/height ratio of 10 cm2/m was proposed as an additional measurement to decide for aortic root surgery and was found to be associated with an increased risk for aortic dissection in several studies. (40-42)
Table 1. Indications of Aortic Root Surgery in Patients with BAV according to Measured Aortic Root Diameter
| Aortic Root Diameter | Indication for Elective Aortic Root Surgery |
|---|---|
| ≥55 mm | All - class I in ACC/AHA guidelines and IIa in ESC guidelines |
| 50-54 mm | If associated with any of:
|
| ≥45 mm | If concomitant valve surgery is indicated |
Conclusions
Bicuspid aortic valve may be complicated with aortic valve stenosis and/or regurgitation, in addition to risk of endocarditis. Furthermore, it is associated with coarctation and aortopathy that may result in aortic aneurysm, dissection or rupture. The definitive treatment is surgery for the valve and/or aortic root, depending on severity of valve lesion, aortic diameter and rate of progression of aortopathy.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.