Background
Coronary slow-flow phenomenon was identified as an exclusive clinical entity in 1972 (1) where the distal opacification of the coronary artery is delayed on angiography in the absence of significant coronary artery disease.
Coronary slow flow phenomenon needs to be differentiated from slow-flow resulting from percutaneous coronary intervention.
Moreover, the clinical profile and presentation of CSFP differs from syndrome X and is also different from coronary slow flow secondary to coronary ectasia or spasm, ventricular dysfunction, valvular heart disease and connective tissue disorders.
Incidence of coronary slow-flow is reported to be 1-7% of all coronary angiograms.
I - Diagnosis
The exact pathogenesis of CSFP is still not clear and is probably multi factorial. Functional and morphological abnormalities in the microvasculature, endothelial dysfunction, raised inflammatory markers, occult atherosclerosis and anatomical factors of epicardial arteries have all been implicated (2).
The diagnosis of the CSFP can be made on the basis of the TIMI flow grade or TIMI frame count (3). TIMI-2 flow grade (ie requiring ≥ 3 beats to opacify the vessel) or a corrected TIMI frame count > 27 frames have been frequently used. The later is based upon images acquired at 30 frames/second and a correction factor of 1.7 for the LAD (4).
Patients with CSFP often present with chest pain and ECG changes. A significant proportion of them present to the emergency department with features of an acute coronary syndrome (5) and may have troponin elevations.
There are case reports of abnormal QT dispersion and ventricular arrhythmias (6).
Affected patients are usually young male smokers.
II - Treatment
Treatment modalities for CSFP are not well established.
The T -type calcium channel blocker mibefradil was evaluated and was found to improve both clinical as well as angiographic outcomes (7). However, due to its many drug to drug interactions, mibefradil is currently not in use. The data on conventional L-type calcium channel blockers use is scarce. Nitroglycerine is of limited value.
In an observational study, Kurtoglu et al found dypiridamole to be useful in the management of CSFP, with symptomatic as well as angiographic improvement (8). Statins with their pleiotropic effects on the vascular function have shown benefit in the treatment of CSFP (9).
Nitric oxide potentiating β-blocker nebivolol improved flow mediated dilatation of brachial artery and controlled chest pain in a study conducted by Albayrak et al (10).
III - Pro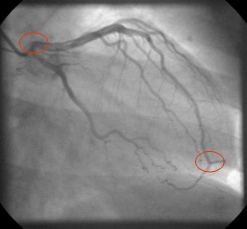 gnosis
gnosis
Coronary slow-flow phenomenon usually has a benign long term outcome but may be associated with relapses. Occasional ventricular arrhythmias and even sudden cardiac death have been reported.
Figure 1: Measurement of coronary flow by CTFC. The speed with which the dye reaches the distal 'pitchfork' bifurcation of LAD from the ostium is measured in frame counts. Normal count is 21 +- 3. A correction factor of 1.7 is used for LAD.
Figure 2: In RCA the flow is measured from ostium to origin of first posterolateral branch. In LCX the flow is measured from ostium to most distal branch of last OM.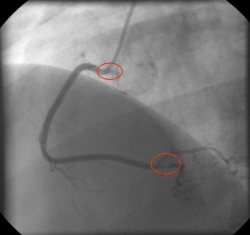
IV - Our Experience
We compared 20 patients diagnosed with CSFP with an equal number of age and sex-matched patients from the same study period, diagnosed as having normal epicardial coronaries and coronary flow. Both groups were similar with respect to smoking status, physical activity, presence of hypertension and diabetes mellitus.
The CSFP group had a higher prevalence of high LDL cholesterol levels (89+ _10.2 Vs 110+_17.5, 'p'< 0.05).
The commonest presentation of CSFP was ACS (65%) requiring hospitalisation;
Fifty-five per cent had ST-T changes on ECG, 15% had +ve Troponins and all patients were managed conservatively. There was no mortality. We concluded that CSFP contributes to significant morbidity with most patients presenting as ACS (11).
Conclusion
Coronary slow flow phenomenon is not an infrequent angiographic finding and contributes to morbidity. Statins and nebivolol show promise for its management but large randomised controlled trials are required for more evidence.



 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.