Introduction
Hypertrophic Cardiomyopathy (HCM) is a condition where there is an increased left ventricular wall thickness or mass, which cannot be solely explained by abnormal loading conditions. Affected patients can experience varying degrees of heart failure and rhythm abnormalities. A subset of individuals may experience sudden cardiac death/arrest SCD/A). HCM can be diagnosed at any age and affects approximately 1:500 of the population. Hence, it is one of the most common rare diseases. Management is tailored to symptom control, device therapy and specific lifestyle advice such as exercise modification to prevent SCD. Recent developments include the availability of disease-modifying therapies in the form of myosin inhibitors to alleviate outflow tract obstruction (Arbelo et al., 2023).
HCM is usually a genetic condition, inherited in an autosomal dominant manner in the majority of cases. This conveys a 50% risk of inheritance for first degree relatives. Therefore, care of the family is part and parcel of the HCM management pathway.
A recent editorial has highlighted the need for holistic care in patients and families impacted by HCM and inequity in service provision across Europe (Olivotto et al., 2025). There is a drive to ensure cardiomyopathy care is included in EU health policy for the optimal implementation of current HCM practice guidelines.
As nurses and allied professionals we can all play a part in ensuring we give the best possible care to our patients impacted by HCM by following these top tips.
Taking a detailed family history
During assessments, it is crucial that we ask specific questions about a patient’s family history. A family history of HCM, cardiac transplantation, early onset heart failure and SCD in a relative <40 y/o would warrant request for further information on these relatives. This will help determine whether further referrals or tests are required to rule out HCM in the patient.
Early referral to a specialist HCM clinic
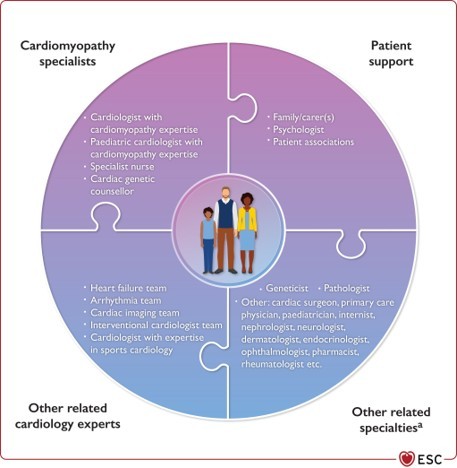
On average, it takes 5.6 years before patients with rare diseases receive a diagnosis and definitive treatment. Current cardiomyopathy guidelines recommend early referral to a specialist inherited cardiac conditions clinic if you suspect an HCM diagnosis to ensure expert evaluation, management and risk stratification by a multi-disciplinary team. Genetic evaluation is also provided which further supports the application precision medicine alongside facilitating advice for first degree relatives. Figure 1 illustrates the typical composition of the multidisciplinary team involved in HCM care.
Figure 1 : Multidisciplinary care of cardiomyopathies, 2023 ESC Guidelines for the management of cardiomyopathies: Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC), Eur Heart J, Volume 44, Issue 37, 1 October 2023, Pages 3503–3626
Supporting patients with lifestyle recommendations
Historically, patients with HCM have been advised not to exercise in order to prevent life-threatening arrhythmias and/or worsening of outflow tract obstruction which leads to collapses/SCD. Updated guidelines now recommend a tailored approach to exercise and physical activity (Pelliccia et al., 2020). The majority of patients are able to partake in mild to moderate exercise which is essential to general health and well-being.
Education and psychological support to empower patients and relatives
Providing comprehensive, evidence-based patient and family education is key to supporting informed consent and shared-decision making (Ingles et al., 2021). Nurses and allied professionals may be involved in aspects of HCM care including implantation of devices, medicines management and genetic counselling. The ability to offer accurate information and space and time for open discussions will ensure clinical care is approached collaboratively with the patient.
Early assessment of psychological needs can ensure early provision of appropriate support. Bereavement counselling and specialist input for post-traumatic stress may be needed in those who have been impacted by a SCD/A.
Signposting to the appropriate patient support groups is also helpful as this provides early peer support and advice for practical adjustments patients often have to make as a result of a diagnosis. Furthermore, as health professionals working with patient groups to support advocacy for HCM, strengthens the voice in policy development and funding for high-quality, equitable services. For example, there is more work to do in ensuring genomic tests are implemented in the standard care pathway.
Supporting research in HCM care
Although advances in cardiovascular genomics are progressing rapidly, there are still gaps in the evidence ranging from refinement of diagnostic and prognostication tools, treatment development to psychological impact and support, and tailoring of cardiac rehabilitation and lifestyle advice (Coats and Fielding, 2024). Whether as nurses and allied professionals we seek to lead research to contribute the scientific evidence or to facilitate recruitment into studies, it is important we are engaged in HCM research to improve care for our patients and to help ensure more diversity and generalisability of research findings.
Conclusion
By adopting these top tips for HCM in our everyday practice as nurses and allied professionals, this will facilitate the shortening of the diagnostic odyssey patients undergo to get to a definitive diagnosis and treatment in one of the most common rare diseases. Having increased knowledge and skill in HCM will also help us manage and support HCM patients and their families in clinical decision making and in adjusting to their condition physically and psychologically. Alongside signposting and working with patient groups, the ambition of holistic care can be achieved.
Author: Doctor Teofila Bueser
Guy's and St Thomas' NHS Trust Foundation Trust, London (United Kingdom of Great Britain & Northern Ireland), ACNAP Education Committee Member 2024-2026, ESC Council on Cardiovascular Genomics Board Member 2024-2026