In the document the clinical diagnosis reviewed and specific recommendations for management of cardiac tamponade are provided. They are briefly listed here:
Recommendation (Clinical Diagnosis):
• Cardiac tamponade should be suspected in patients presenting with hypotension, jugular venous distension, pulsus paradoxus, tachycardia, tachypnea and/or severe dyspnea;
• Additional signs may include low QRS voltages, electrical alternance, enlarged cardiac silhouette on chest X ray.
Recommendation (Imaging):
• Echocardiography is the diagnostic method of choice in suspected cardiac tamponade and should be carried out without delay.
• CT and CMR are not part of the routine evaluation of patients with suspected cardiac tamponade, they are useful to rule out concomitant diseases involving the mediastinum and lungs in patients with large pericardial effusions (i.e. cancer or aortic dissection).
Recommendation (Differential Diagnosis):
• Differential diagnosis should include constrictive pericarditis, congestive heart failure, and advanced liver disease with cirrhosis.
Recommendation (indication for drainage):
• Pericardial drainage is indicated for each case with established diagnosis of cardiac tamponade. If the patient is hemodynamically stable the procedure should be performed within 12-24 hours from diagnosis, after obtaining laboratory results including the blood counts.
• Indications for urgent surgical treatment of cardiac tamponade include hemopericardium due to type A aortic dissection, ventricular free wall rupture in acute myocardial infarction, trauma, or purulent effusion in unstable septic patients, and loculated effusions that can not be managed percutaneously.
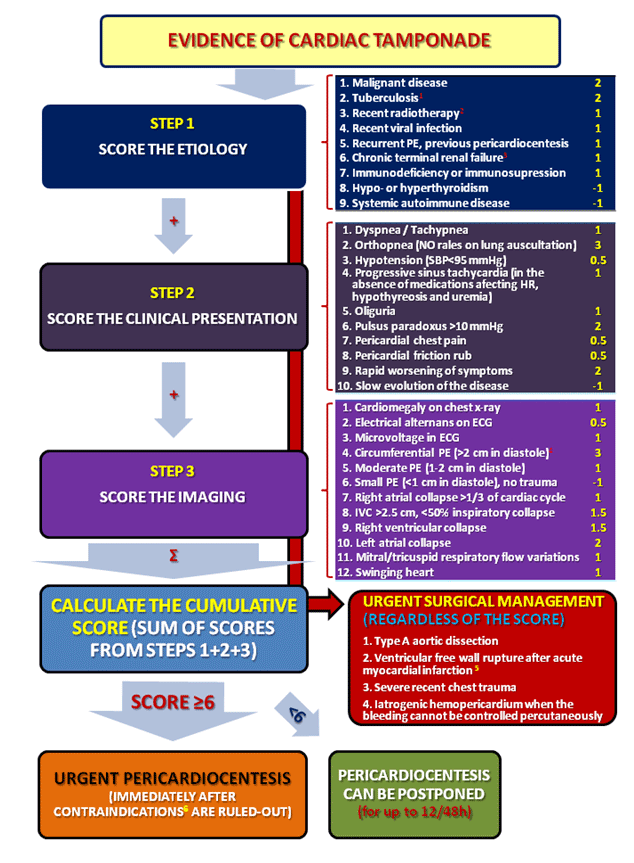
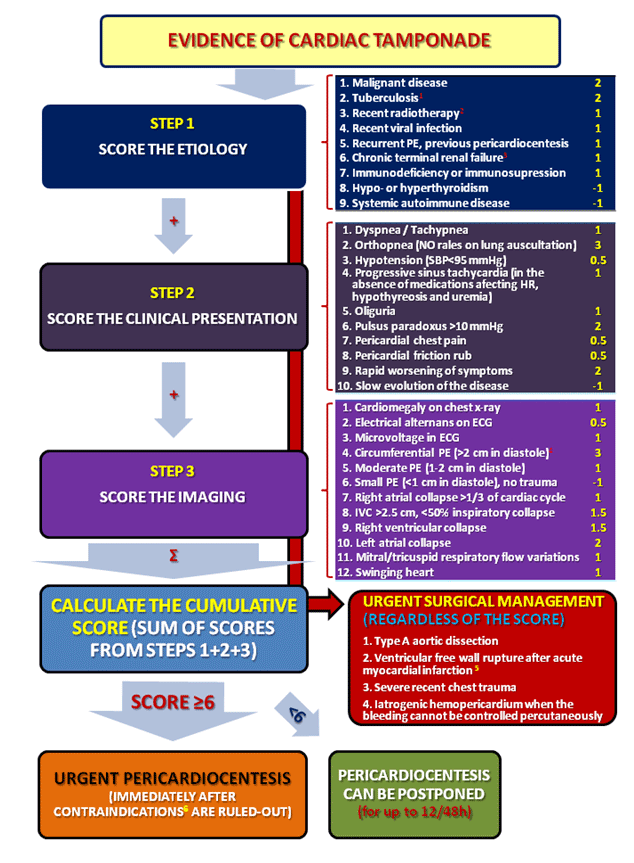
• In patients with cardiac tamponade a stepwise scoring system may be useful for the triage of patients (Figure). A total score ≥6 warrants immediate pericardiocentesis in the absence of contraindications. In rapidly deteriorating patients with iatrogenic hemopericardium or any other very unstable patient pericardial drainage should be performed without any delay for laboratory tests but treating anticoagulation (protamine), prolonged INR (fresh frozen plasma) and/or anemia (plasma-free blood transfusion) simultaneously with the drainage of the pericardium.
Recommendation (Guidance for pericardiocentesis):
• Echocardiography is mandatory to guide pericardiocentesis and select the approach (intercostal vs. subxiphoid), except in case of life threatening tamponade.
• Fluoroscopy can be considered for early diagnosis and rescue pericardiocentesis especially for iatrogenic effusions after specific interventional techniques (i.e. radiofrequency ablation, other percutaneous interventions), although echocardiography should be immediately available as well.
Recommendation (Prolonged drainage):
• Drainage of more than 1 liter effusion from the pericardial space should be avoided and prolonged catheter drainage should be provided for the remaining effusion
• Prolonged pericardial drainage can be discussed in selected cases, especially for the management of neoplastic effusions, in order to prevent recurrence of tamponade.
Urgent pericardiocentesis or drainage of pericardial effusion is indicated for each patient with established diagnosis of cardiac tamponade and hemodynamic shock. The decision to drain an effusion and to do it immediately, urgently or schedule the procedure electively must take into account the clinical presentation, changes in the hemodynamic status over time (in the range of several minutes to several hours depending on the aetiology), the risk-benefit ratio of the procedure and the echocardiographic findings.
Since cardiac tamponade can develop slowly, and the symptoms and signs are neither highly sensitive nor specific, Halpern et al. (2) introduced a scoring index to guide the decision for pericardial drainage, based on effusion size, echocardiographic assessment of hemodynamics, and clinical factors. On the basis of currently available data, and the consensus of experts we propose a new stepwise scoring system for the triage of patients requiring pericardiocentesis (Figure). The scoring system should be applied for the triage cardiac tamponade without haemodynamic shock, where immediate pericardiocentesis is mandatory and life saving.
Recommendation (Clinical Diagnosis):
• Cardiac tamponade should be suspected in patients presenting with hypotension, jugular venous distension, pulsus paradoxus, tachycardia, tachypnea and/or severe dyspnea;
• Additional signs may include low QRS voltages, electrical alternance, enlarged cardiac silhouette on chest X ray.
Recommendation (Imaging):
• Echocardiography is the diagnostic method of choice in suspected cardiac tamponade and should be carried out without delay.
• CT and CMR are not part of the routine evaluation of patients with suspected cardiac tamponade, they are useful to rule out concomitant diseases involving the mediastinum and lungs in patients with large pericardial effusions (i.e. cancer or aortic dissection).
Recommendation (Differential Diagnosis):
• Differential diagnosis should include constrictive pericarditis, congestive heart failure, and advanced liver disease with cirrhosis.
Recommendation (indication for drainage):
• Pericardial drainage is indicated for each case with established diagnosis of cardiac tamponade. If the patient is hemodynamically stable the procedure should be performed within 12-24 hours from diagnosis, after obtaining laboratory results including the blood counts.
• Indications for urgent surgical treatment of cardiac tamponade include hemopericardium due to type A aortic dissection, ventricular free wall rupture in acute myocardial infarction, trauma, or purulent effusion in unstable septic patients, and loculated effusions that can not be managed percutaneously.
• In patients with cardiac tamponade a stepwise scoring system may be useful for the triage of patients (Figure). A total score ≥6 warrants immediate pericardiocentesis in the absence of contraindications. In rapidly deteriorating patients with iatrogenic hemopericardium or any other very unstable patient pericardial drainage should be performed without any delay for laboratory tests but treating anticoagulation (protamine), prolonged INR (fresh frozen plasma) and/or anemia (plasma-free blood transfusion) simultaneously with the drainage of the pericardium.
Recommendation (Guidance for pericardiocentesis):
• Echocardiography is mandatory to guide pericardiocentesis and select the approach (intercostal vs. subxiphoid), except in case of life threatening tamponade.
• Fluoroscopy can be considered for early diagnosis and rescue pericardiocentesis especially for iatrogenic effusions after specific interventional techniques (i.e. radiofrequency ablation, other percutaneous interventions), although echocardiography should be immediately available as well.
Recommendation (Prolonged drainage):
• Drainage of more than 1 liter effusion from the pericardial space should be avoided and prolonged catheter drainage should be provided for the remaining effusion
• Prolonged pericardial drainage can be discussed in selected cases, especially for the management of neoplastic effusions, in order to prevent recurrence of tamponade.
Urgent pericardiocentesis or drainage of pericardial effusion is indicated for each patient with established diagnosis of cardiac tamponade and hemodynamic shock. The decision to drain an effusion and to do it immediately, urgently or schedule the procedure electively must take into account the clinical presentation, changes in the hemodynamic status over time (in the range of several minutes to several hours depending on the aetiology), the risk-benefit ratio of the procedure and the echocardiographic findings.
Since cardiac tamponade can develop slowly, and the symptoms and signs are neither highly sensitive nor specific, Halpern et al. (2) introduced a scoring index to guide the decision for pericardial drainage, based on effusion size, echocardiographic assessment of hemodynamics, and clinical factors. On the basis of currently available data, and the consensus of experts we propose a new stepwise scoring system for the triage of patients requiring pericardiocentesis (Figure). The scoring system should be applied for the triage cardiac tamponade without haemodynamic shock, where immediate pericardiocentesis is mandatory and life saving.

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.