The CORE320 study is a prospective multicentre international trial which evaluated the diagnostic accuracy of combined non-invasive CTA and CTP as compared with invasive angiography (ICA) and single photon computed tomography myocardial perfusion imaging (SPECT-MPI). The primary objective was to determine whether combined noninvasive CTA and CTP could reliably determine the presence or absence of flow limiting coronary stenoses as defined by the combination of ICA and SPECT-MPI.
Patients between 45 and 85 years of age with suspected or known coronary artery disease and clinically referred for ICA were eligible for participation. The study enrolled 436 patients, of whom 381 successfully completed all imaging at 16 centers in eight countries (Canada, USA, Brazil, the Netherlands, Germany, Denmark, Japan, and Singapore).
The study design included four imaging components: CTA, stress CTP, ICA, and SPECT-MPI, as displayed in the Figure below. Images were evaluated in double blinded core laboratories. The area under the receiver operating characteristic curve (AUC) was used as the primary diagnostic parameter. The study was sponsored by Toshiba Medical Systems.
Sixty-six percent of the study participants were male, the median (interquartile range [IQR]) age was 62 [56,68], body mass index 27 [24,30], and Agatston calcium score 162 [9, 530]. Participants had a history of traditional risk factors for coronary artery disease - 34% were diabetic, 26% had a history of previous myocardial infarction, 29% had prior percutaneous coronary intervention, 78% were positive for hypertension, 68% were positive for dislipidemia, and 45% had a family history of coronary artery disease.
The prevalence of obstructive coronary artery disease defined by combined ICA and SPECT/MPI was 38% and for ICA alone 59%. The patient-based diagnostic accuracy (AUC) of combined CTA and CTP for detecting or excluding flow-limiting CAD was 0.87 (95% CI 0.83-0.91), and 0.89 (95% CI 0.86-0.93) when the ICA stenosis reference standards were =50% and =70% respectively. CTP increased the diagnostic accuracy of CTA alone to delineate flow-limiting disease (AUC 0.87 [95%CI 0.83-0.91] vs. 0.81 [95%CI 0.77-0.86], respectively, p<0.001). The combination of CTA and CTP had similar diagnostic power to the combination of ICA and SPECT-MPI in identifying revascularised patients at 30-days.
"We found the addition of CT myocardial perfusion to CT angiography allows clinicians to distinguish between anatomic and flow limiting stenoses in patients with suspected coronary artery disease," said Dr Lima.
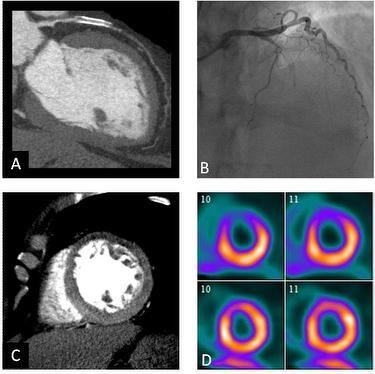
An example case of the four study imaging components. Panel A depicts a CTA image with a 100% lesion in the left anterior descending artery. Panel B depicts an ICA image with a 100% lesion in the left anterior descending artery. Panel C depicts a CTP image with defects read in basal anterior (severe), distal anterior (severe), distal anteroseptal (moderate), and apex (moderate). Distal anterior and apical defects had fixed components.
Panel D: SPECT perfusion defects read in distal anterior (severe), distal anteroseptal (severe), and apex (severe). Disatal anterospetal defect fixed.
ENDS

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.