The case
Description
- 19 year-old Afro-Caribbean male athlete.
- It was performed as part of familial evaluation after his 16-year-old brother died suddenly whilst skateboarding.
- Subsequent autopsy identified features suggestive of arrhythmogenic right ventricular cardiomyopathy (ARVC).
Question
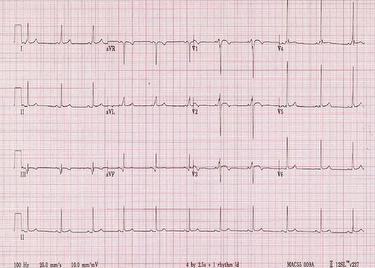
What findings does the ECG demonstrate?
Answer
- Short PR-interval with associated delta wave.
- T-wave inversion in leads V1-V3 with associated convex ST-segment elevation.
- Suspicion of early repolarisation pattern in leads V5 and V6.
- Voltage criterion for left ventricular hypertrophy.
Discussion
The ECG demonstrates features suggestive of an accessory pathway. Evidence of an accessory pathway can be present in up to 0.3% of individuals during routine ECG, the great majority being asymptomatic. Although they have been associated with sudden cardiac death in both athletic and non-athletic individuals, they are not inherited in the great majority of cases. In this particular case electrophysiological studies identified a slow conducting accessory pathway in the right free wall.
The presence of anterior T-wave inversions with convex ST-segment elevation is present in 12% of Afro-Caribbean athletes and is considered a manifestation of ethnic variation to physiological adaptation to exercise. In the presence of symptoms or family history of cardiomyopathy or sudden cardiac death however, all athletes should undergo comprehensive clinical evaluation to exclude quiescent cardiomyopathy and in particular ARVC.
In this case given the family history both the athlete and all his 1st-degree family relatives were comprehensively evaluated. The mother also exhibited T-wave inversions in the anterior leads. Subsequent gene testing confirmed the presence of a pathogenic desmosomal protein mutation in both the athlete and his mother, most likely accounting for the sudden cardiac death.
Based on a clinical diagnosis of ARVC, confirmed by genetic testing, the athlete would not be eligible for formal competition, according to the ESC recommendations*.
Further treatment is dictated by the presence of arrhythmia and associated haemodynamic compromise. High risk individuals such as individuals with prior cardiac arrest, episodes ventricular tachycardia with haemodynamic compromise (syncope) should be offered an implantable cardioverter defibrillator (ICD).
Voltage criterion for left ventricular hypertrophy is common in athletes and in isolation it is rarely associated with underlying disease.
Finally, early repolarisation patterns are common in athletes and do not indicate pathology, particularly when associated with an up-sloping ST-segment.
Interested in learning more?
Access the ESC e-learning platform and discover the EAPC Sports Cardiology online courses.
Not yet an EAPC member?
Note: The views and opinions expressed on this page are those of the author and may not be accepted by others. While every attempt is made to keep the information up to date, there is always going to be a lag in updating information. The reader is encouraged to read this in conjunction with appropriate ESC Guidelines. The material on this page is for educational purposes and is not for use as a definitive management strategy in the care of patients. Quiz material in the site are only examples and do not guarantee outcomes from formal examinations.

 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.