Hypokalemia and the heart
Potassium is the most abundant intracellular cation and is necessary for maintaining a normal charge difference between intracellular and extracellular space. Potassium homeostasis is important for normal cellular function and is regulated by ion-exchange pumps (primarily cellular, membrane-bound, sodium-potassium ATPase pumps). Derangements of potassium regulation often lead to neuromuscular, gastrointestinal and cardiac rhythm abnormalities.
The normal level of plasma potassium is 3,8 – 5,1 mmol/l. The deviations to both extremes (hypo- and hyperkalemia) are related to the risk of cardiac arrhythmias. Potassium levels below 3,0 mmol/l cause significant Q-T interval prolongation with subsequent risk of torsade des pointes, ventricular fibrillation and sudden cardiac death. Potassium levels above 6,0 mmol/l cause peaked T waves, wider QRS komplexes and may result in bradycardia, asystole and sudden death. Hyperkalemia is most frequently caused by renal failure (frequently a trigger is suboptimal drug therapy, e.g. spironolactone or other potassium-sparing diuretics and/or angiotensin-converting enzyme inhibitor, or even potassium supplementation therapy) or by hemolysis and will not be the subject of this article, which is focused on hypokalemia.
Hypokalemia usually occurrs as a complication of certain illnesses or medications. Interestingly, it was shown that 'modern' food has significantly decreased potassium content. As a result, the tendency towards mild hypokalemia is rather frequent among healthy subjects. This can be easily corrected by the change of food habits – i.e. increase in fresh fruit and vegetable intake. The possible causes of hypokalemia are listed in Table 1.
Table 1: Possible Causes of Hypokalemia
| Diuretics |
| Laxatives |
| Gastrointestinal losses (diarrhoea, vomiting) |
| Prolonged excess of caffeine |
| Long-term inadequate intake |
| Other drugs (theofylline, aminophylline, caffeine, verapamil, amphotericin B, ampicillin, cerbenicillin, high-dose penicillin, amphetamin, aminoglykosides) |
| Corticosteroid therapy, Cushing's syndrome |
| Hyperthyroidism |
| Hyperaldosteronism |
| Diabetic ketoacidosis |
| Alkalosis |
| Hyperhydration |
| Hypothermia |
| Periodic hypokalemic paralysis |
| Renal tubular disorders (distal renal tubular acidosis, Bartter syndrome, Gitelman syndrome) |
| Catecholamines, sympatomimetics |
| Cystic fibrosis |
| Insulin |
| Hypomagnesemia |
The clinical manifestations of hypokalemia include gastrointestinal hypomotility or ileus, muscle weakness or cramping.
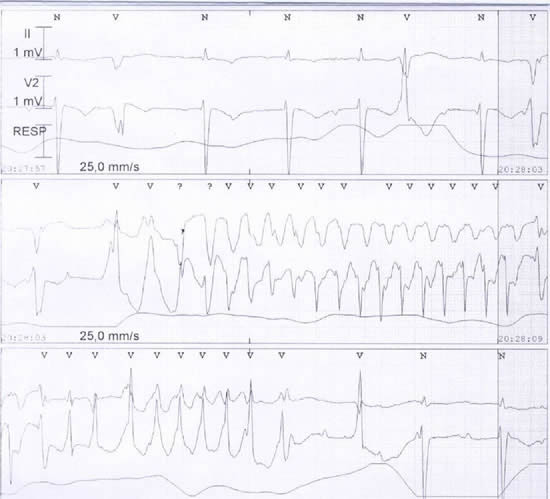
The most dangerous aspect of hypokalemia is the risk of ECG changes (QT prolongation, appearance of U waves that may mimic atrial flutter, T-wave flattening, or ST-segment depression) resulting in potentially lethal cardiac dysrhythmia. The pro-arrhythmic risk of hypokalemia is significantly increased when hypokalemia occurs simultaneously with other pro-arrhythmic settings (Table 2).
Table 2: Diseases / Situations Potentially Contributing to the Pro-Arrhythmic Risk of Hypokalemia.
| Antiarrhythmic drugs class I or III |
| Digitalis |
| Left ventricular dilatation |
| Left ventricular hypertrophy |
| Ischemia |
| Q-T prolongation |
| Excess caffeine |
| Stress, exhaustion |
| Post-operative setting |
ECG findings in hyperkalemia:
Kalium cca > 6 mmol/l: Tall peaked symmetrical T waves in all leads, mainly visible in V2-4. The QT interval is shorter.
Kalium cca 7-8 mmol/l: Prolongation of the PQ interval, flattening of the P wave.
Kalium cca 8-10 mmol/l: QRS complex deformities (widening), resulting in asystole or more rarely in ventricular fibrillation.
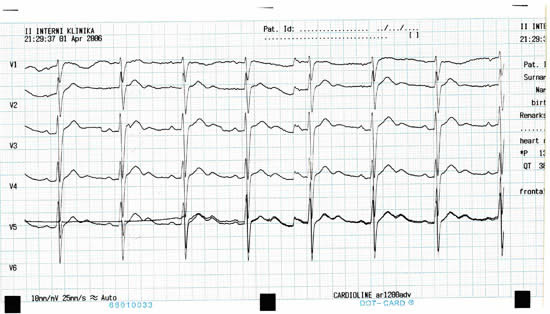
ECG findings in hypokalemia:
Kalium cca 3,0–3,8 mmol/l: Flattening or inversion of T waves.
Kalium cca 2,3 –3,0 mmol/l: Q-T interval prolongation (longer duration of the T wave), visible U wave, mild ST depression (0,5 mm), ventricular extrasystoles.
Kalium cca < 2,3 mmol/l: torsades de pointes, ventricular fibrillation.
Therapy of hypokalemia
The treatment of hypokalemia depends on its severity and etiology. Unlike hyponatremia, in which the total body sodium deficit can be readily estimated, serum potassium may not accurately reflect total body stores. During diabetic ketoacidosis, serum potassium levels may be initially elevated, even when severe depletion of total body potassium is present. Correction of acidosis in diabetic ketoacidosis may cause a precipitous drop in serum potassium levels. Transient, asymptomatic, or mild hypokalemia may spontaneously resolve or may be treated with enteral potassium supplements. Symptomatic or severe hypokalemia should be corrected with a solution of intravenous potassium: 10-40 mEq infused over two to three hours (infusion rate should not to exceed 40 mEq/h). In less urgent situations, oral supplementation is preferred and safer: 50-100 mEq/d divided two-four times per day. Larger doses may be needed in severe depletion to replenish potassium body storage.
Long-term treatment should be based on the recognition of the hypokalemia cause. When this cause (e.g. drug effect – most frequently diuretics) can be corrected, no other long-term treatment is needed. The oral drugs leading to increases of potassium levels are potassium-sparing diuretics (spironolactone, amiloride), potassium chloride tablets, and ACE inhibitors. These drugs must always be used with caution to avoid hyperkalemia, which may be as dangerous as hypokalemia.
Conclusion:
Hypokalemia is a frequent disorder, especially important in cardiac patients. While in patients without heart disease hypokalemia rarely leads to death, among cardiac patients (who have inherent risk for arrhythmias and who frequently use medications potentially augmenting the risks of hypokalemia and/or arrhythmia) unrecognized hypokalemia may be one of the leading causes of iatrogenic mortality. As far as hyperkalemia also carries substantial risk, it is of utmost importance for a practicing cardiologist to keep the potassium levels within normal limits in all cardiac patients.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.