Aortic aneurysms carry a risk of acute aortic dissection or rupture in the absence of surgical treatment. Indeed aortic dissections or ruptures are the 13th cause of death in Western countries (1, 2). Their incidence is estimated at around 4.5 per 100 000 persons. Aneurysms of the ascending aorta make up for more than half of all thoracic aneurysms (1-3), with men being affected more than women. Aortic aneurysms carry a risk of acute aortic dissection or rupture in the absence of surgical treatment. Indeed aortic dissections or ruptures are the 13th cause of death in Western countries (1, 2). Their incidence is estimated at around 4.5 per 100 000 persons. Aneurysms of the ascending aorta make up for more than half of all thoracic aneurysms (1-3), with men being affected more than women.
Aortic aneurysms carry a risk of acute aortic dissection or rupture in the absence of surgical treatment. Indeed aortic dissections or ruptures are the 13th cause of death in Western countries (1, 2). Their incidence is estimated at around 4.5 per 100 000 persons. Aneurysms of the ascending aorta make up for more than half of all thoracic aneurysms (1-3), with men being affected more than women.
Aortic aneurysms carry a risk of acute aortic dissection or rupture in the absence of surgical treatment. Indeed aortic dissections or ruptures are the 13th cause of death in Western countries (1, 2). Their incidence is estimated at around 4.5 per 100 000 persons. Aneurysms of the ascending aorta make up for more than half of all thoracic aneurysms (1-3), with men being affected more than women.
Types of Aortic aneurysms
Aortic aneurysms can be classified to 2 distinct types:
1. Aortic root aneurysms (figure 1): the dilatation of the aorta involves the initial portion of the aorta and includes the sinuses of Valsalva. They may be associated with connective tissue disorders (e.g. Marfan’s Syndrome) and patients are usually young (30-50 yrs).Their management often includes replacement or repair of the aortic valve.
2. Supravalvular aortic aneurysms (figure 2): these involve the ascending thoracic aorta above the sinuses of Valsalva. The main aetiological process is atherosclerotic disease thus patients are usually older (55-70 yrs). Their treatment does not necessarily incorporate a valvular procedure (2).
Progression and natural history of ascending aortic aneurysms
The average annual growth of ascending aortic aneurysms is 1–4 mm. However, this rate is greater in patients with Marfan’s syndrome or with bicuspid valves. Larger aneurysms also grow at a faster rate. Other factors that contribute to accelerated dilatation are smoking, high blood pressure, renal failure, male sex, fibrocalcific changes in the aortic valve, and left ventricular wall motion abnormalities (2). When the aorta reaches 6 cm in size, reported yearly rates of rupture, dissection, and death are 3.6%, 3.7%, and 10.8%, respectively (4).
Clinical Presentation
Most aneurysms have a long latent period before clinical symptoms appear. Diagnosis is thus established incidentally in many cases during an imaging examination on the chest (chest XR, echocardiography…etc.). Symptoms from compression of adjacent structures can be the presenting feature: chronic chest pain, cough, dysphagia can result from pressure on the sternum, trachea or oesophagus respectively. However in 75% of patients, the first presentation is with acute sudden severe tearing chest pain. This is highly suggestive of imminent rupture or aortic dissection and requests urgent medical care.
Diagnosis is confirmed by echocardiography which also evaluates valvular competency. CT scan with injection of contrast material together with 3D reconstruction permits accurate measurement of the aortic diameters and to establish reference values for follow up (figure 3). MRI offers similar diagnostic facilities. Aortography is only performed if a surgical intervention is being planned and should incorporate coronary artery angiography as part of preoperative work up.
Treatment
Conservative management
ß-blockers are indicated in asymptomatic patients during the follow up period for patients not requiring surgery. Their negative inotropic and chronotropic effects decrease the rate and rise of the arterial pulse with a delay in aortic root dilatation and have been shown to improve survival particularly in patients with Marfan’s syndrome (5,6). Since aortic aneurysms can be hereditary, a detailed family history and evaluation of other family members should be carried out.
Surgery:
Surgical intervention is performed under cardiopulmonary bypass through median sternotomy. The overall indications for surgery are cited in table 1. Immediate and emergency surgery is indicated in patients with acute rupture or dissection of the aortic aneurysm and evidently, is associated with considerable morbi-mortality (30 % vs. 4.3% in emergency versus elective surgery, respectively) (7). These high figures of morbi-mortality associated with emergency surgery highlight the importance of prior diagnosis and meticulous follow up.
The decision to perform elective surgery is directly related to the progression of the aortic diameter and the aetiology of the aneurysm (6,8). Table 2 summarises the current French, American and European guidelines for the indication of surgery in aneurysms of the ascending thoracic aorta.
Supravalvular aneurysms can be treated by a simple supracoronary tube graft (figure 4), whereas aortic root aneurysms need a Bentall (incorporating an aortic valve replacement) or valve sparing procedure with reimplantation of the coronary ostia which are found within the diseased zone.
The choice of the surgical technique depends on the type of the aneurysm, aetiology, patient life expectancy and the presence of contraindications to anticoagulation.
Table 1. Indications for surgery
1. Aneurysms with greatest diameter > 55 mm measured by CT scan with injection of contrast material or MRI.
2. Symptomatic aortic regurgitation.
3. History of systemic embolism from a mural thrombus.
4. Symptoms from compression of adjacent structures.
5. Rupture or acute aortic dissection.
Table 2 :Current French, American and European guidelines for the indication of surgery in aneurysms of the ascending thoracic aorta
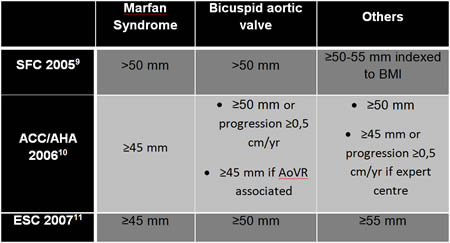
Figure 1. Aortic root aneurysm

Figure 2. Supralvular aortic aneurysm
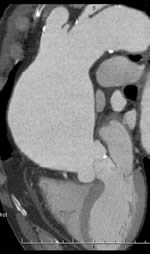
Figure 3. CT scan with injection of contrast material and 3D reconstruction

Figure 4: Surgical replacement of the ascending aorta by Dacron tube. (LV: left ventricle, RA : right atrium)
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.
Conclusion:


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.