The presence and the extent of late gadolinium enhancement by cardiac Magnetic Resonance predict adverse outcomes in non ischemic cardiomyopathy and represent an arrhythmogenic substrate in hypertrophic cardiomyopathy. The role of cardiovascular MRI is changing from the mere potentiality toward the clinical use to improve risk stratification strategies. Patients affected by dilated non-ischemic cardiomyopathy or hypertrophic cardiomyopathy often represent a clinical dilemma on the therapeutical point of view. While in the whole population a risk stratification is possible, in the individual patient the outcome is unpredictable and current risk stratification approaches are sub-optimal.
Recently, the introduction of a new imaging procedure (late gadolinium enhancement by cardiac Magnetic Resonance(MR)) has made possible the detection of intramyocardial fibrosis which is variably represented either in non-ischemic dilated cardiomyopathy (30-40% of patients) and in hypertrophic cardiomyopathy (60-70%). In a paper on 101 patients affected by dilated cardiomyopathy (1) midwall fibrosis was present in 35% of patients and was associated with a higher rate of the predefined primary combined end point of all-cause death and hospitalization for a cardiovascular event independently from ventricular remodelling. In addition, midwall fibrosis by cardiac MR predicted sudden cardiac death and ventricular tachicardia.
In another prospective cohort study 65 patients affected by non ischemic cardiomyopathy (2) with left ventricular ejection fraction < or = 35% , the patient with evidence of fibrosis at cardiac MR had an 8-fold higher risk of experiencing major cardiac event (hospitalization, appropriate implantable cardioverter-defibrillator firing and cardiac death). Also hypertrophic cardiomyopathy seems to have in cardiac fibrosis, as detected by cardiac MR a powerful predictor of events and namely of tachyarrhythmias. In a study on 177 patients affected by this disease (3), those (60%) with evidence of fibrosis showed a greater likehood and increased frequency of ventricular tachyarrhythmias (including non sustained ventricular tachycardia).
These prospective results point out the relevance of fibrosis as a pathophysiological substrate to be integrated with the clinical and the other imaging findings systematically collected in the majority of patients affected by cardiomyopathy despite differences in the pathological substrate.
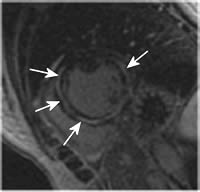
Figura1
Image in short axis of the left ventricle obtained in a patient with non-ischemic dilated cardiomyopathy. Inversion Recovery Gradient Echo image.
Late gadolinium enhancement. Arrows show the presence of a midwall accumulation of the contrast agent which can be interpreted as myocardial fibrosis.
Conclusion:
At this stage of knowledge cardiologists would have to consider always the possibility to assess the presence of fibrosis as an adjunctive parameter to evaluate the risk of the individual patient affected by dilated or hypertrophic cardiomyopathy.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.