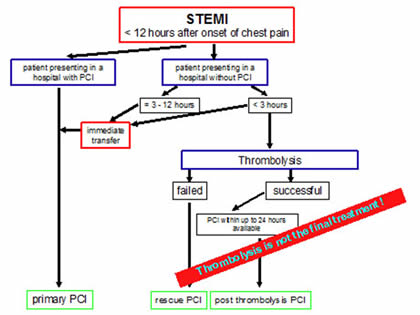
1 STEMI : Treatment remains the same
Current guidelines recommend PCI as the most effective treatment after PCI.
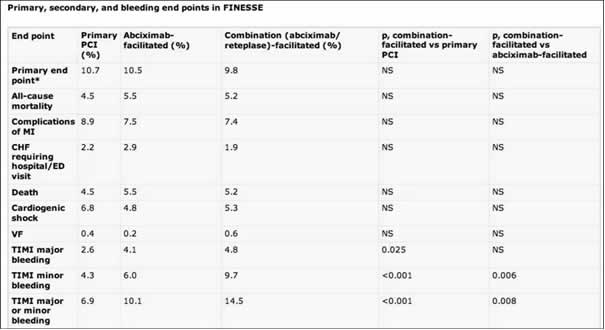
Finesse Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events aimed at determining if additional pharmacological interventions before PCI, could improve outcomes.
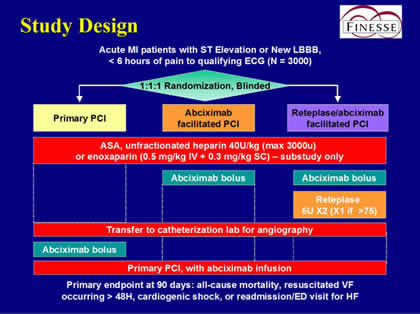
This trial, found no difference in the primary endpoint of death, cardiogenic shock, heart failure, or resuscitated ventricular fibrillation by 90 days between the 3 groups. There was also no difference in the components of the primary endpoint.
The take-home message for patients with STEMI is that:
If a patient, shows up in your practice or ambulance with STEMI, you should
- immediately administrate Acetyl Salicylic Acid i.v.
- clopidogrel loading dose of 600 mg
- do not give Abciximab or other GP IIb/IIIa Inhib., no thrombolysis, if cathlab can be reached within 90 to 120 minutes.
Regarding the specific study of the best treatment for women with NSTE ACS, The Michelangelo study aimed at determining the best approach, given this background:
- women with NSTE ACS have less severe CAD and a better prognosis than men.
- some treatments (eg LMWH or CABG surgery) are associated with a higher risk in women. Others (GPIIB/IIIa inhib) appear ineffective.
- randomised trials of routine invasive strategy in NSTE ACS show benefits in men but the results in women are contradictory.
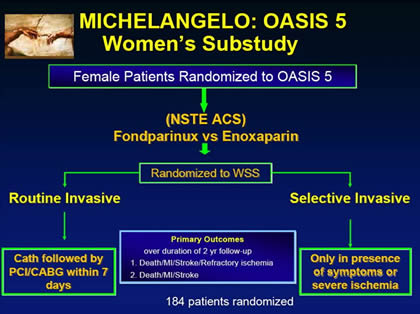
In this study, women with NSTE ACS did not benefit from a routine invasive strategy.
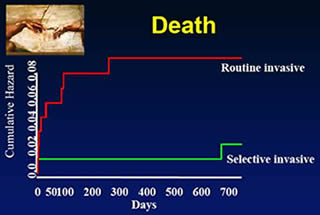
On the contrary, patients randomised to a routine invasive strategy had a higher mortality rate.
The results taken together with the results of previous larger trials suggest that the results from men do not necessarily apply to women and large scale randomised trials in women are needed to determine the optimal strategy in NSTE ACS.
2 Drug-Eluting stents: they do not increase mortality
Using data from the Swedish Coronary Angiography and Angioplasty Registry the Long-Term Outcomes with Drug-Eluting Stents versus Bare-Metal Stents in Sweden evaluated 6033 patients treated with drug-eluting stents and 13,738 patients treated with bare-metal stents in 2003 and 2004.
Drug-eluting stents were associated with an increased rate of death, as compared with bare-metal stents. However, in 2005, the trend began to change, with drug-eluting stents starting to get better results than BMS.

And better restenosis rates with DES, as well.
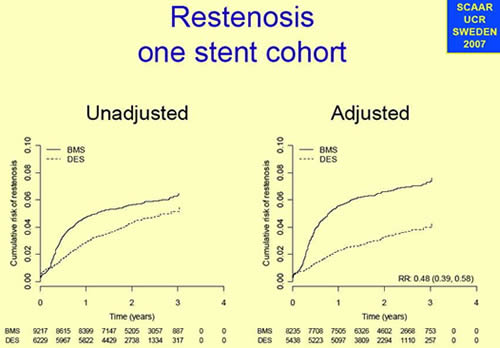
The conclusions were that
During 4 years follow-up the DES-group compared to the BMS-group, with adjustment for differences in available background characteristics, showed:
- no overall significant difference in mortality of myocardial infarction
- a significantly lower event rate during the initial 6 months
- a significantly higher event rate after 6 months which is compensated by the lower early event rate
- a relative reduction of restenosis by almost 50%
corresponding to an absolute reduction of 6.5%
The take-home message for DES is
- drug-eluting stents do not increase mortality
- they reduce the need for reinterventions and therefore improve the quality of life of patients
- There is no class-effect of DES
- Many of the CE-approved DES has never been tested in randomised studies
3 – Secondary prevention – lacking
Euroaspire Surveys I, II and III have interviewed and examined 8457 patients in eight countries first in the early 1990s, then in 2000 and in 2006-2007. Between the first and third survey, it has found:
- increased smoking in those under age 50 and in women
- increased overweight from 25% to 38%
- increased central obesity from 42% to 54%
- increased diabetes from 17 to 28%
Despite increased use of anti-hypertensive medication, those reaching therapeutic targets fell from 41% to 39% - making for 61% above therapeutic target.
The only positive data is the continuing improvement in lipid control with increased use of statins.
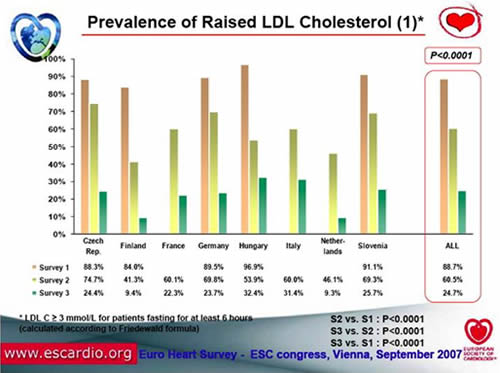
The conclusions to draw from Euroaspire are that Lifestyle of coronary patients is a major cause for concern with no change in prevalence of smoking and continuing adverse trends in the prevalence of obesity and central obesity.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.