Beta-blockers are well known to be effective in the treatment of arterial hypertension, coronary artery disease, tachyarrhythmias arterial hypertension and heart failure. Their predominant mechanism of action, i.e., the inhibition of the stimulation of sympathetic beta-adrenoceptors by adrenaline and noradrenaline, is well known all around. and the significant benefits from beta-blockers in reducing cardiovascular end-points result from beta1-blockade.1 Since intrinsic sympathomimetic activity (ISA) detracts from efficacy, beta-blockers with ISA (particularly pindolol, xamoterol and bucindolol) have performed poorly in reducing morbidity and mortality.1 Therefore, beta-blockers with ISA cannot be recommended per se, and this article refers to beta-blockers without ISA.
However, there is still a number of marked differences between “the members of the family of beta-blockers”, first of all the fact that there are actually “three generations of beta-blockers” (Table 1), with the 1st generation being non-selective, the 2nd generation being beta1-selective (“cardioselective”), and the 3rd generation showing additional vasodilating effects.
I - Three generations of beta-blockers
1) Accordingly, 1st generation beta-blockers
- should be used only in patients with particular additional indications such as hyperthyrosis or portal hypertension (propranolol) or special arrhythmias (sotalol) where these two substances have been shown to be particularly effective due to their additional effects on top of beta-blockade.
2) Substances of the 2nd generation
- should be given preferably in patients with coronary artery disease (particularly following myocardial infarction), tachyarrhythmias and/or heart failure, but they may also be useful in arterial hypertension.
However, the latter especially obviously does not hold true for atenolol since it has been shown in a large meta-analysis2 that this drug caused significantly higher mortality than other active treatments whereas non-atenolol beta-blockers showed a (non-significant) tendency to decrease both mortality and myocardial infarction compared to other antihypertensives.2 Therefore, the authors concluded: “Our results cast doubts on atenolol as a suitable drug for hypertensive patients. Moreover, they challenge the use of atenolol as a reference drug in outcome trials in hypertension.”
Unfortunately, most outcome studies in arterial hypertension showing other antihypertensives being “better” than beta-blockers used atenolol as a reference drug. Neverheless,
- other beta-blockers of the 2nd generation, especiallly metoprolol and bisoprolol, still remain indicated particularly in the treatment of coronary artery disease, tachyarrhythmias and heart failure since they never were shown to share these disadvantages with atenolol.
Due to their additional vasodilating effects Beta-blockers of the 3rd generation are particularly useful in patients with arterial hypertension and/or heart failure. However, beta-blockers have been questioned in the treatment of arterial hypertension since they may cause metabolic side effects, whereas this obviously does not hold true for the 3rd generation. Accordingly, the 2007 Guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of, Cardiology4,5 emphasise that “this may not apply, however, to vasodilator beta-blockers, such as carvedilol and nebivolol, which have less or no metabolic action, as well as a reduced incidence of new onset diabetes compared with classical beta-blockers.” Indeed, it has been shown that nebivolol rather decreases than increases the incidence of new onset diabetes compared to placebo6 and carvedilol shows rather favourable metabolic effects such as an increase of the insulin sensitivity index and a decrease in triglyceride plasma concentrations7. Therefore, in this context
3) 3rd generation beta-blockers
carvedilol and nebivolol clearly differ from the those of the 1st and 2nd generation since they
- do not show unfavourable metabolic side effects.
II – 4 “special beta-blockers”
Finally, please find a short overview of four “special beta-blockers” featuring particular additional effects (table 2):
1) Nebivolol
is one of the “youngest members” of the family of beta-blockers widely used in clinical practice. Actually, nebivolol appears to be the drug with the highest beta1-selectivity8. However, this has been questioned by other authors.9 In addition, nebivolol causes NO-derived vasodilation which has been shown in humans by a marked increase in forearm blood flow that can be completely abolished by coinfusion of L-NMMA, a specific inhibitor of NO-synthase.10 This vasodilating effect has clinical relevance since it has been shown that the beta-blocking potency of 5 mg nebivolol is comparable to that of 25 mg atenolol, whereas the blood pressure lowering effect of 5 mg nebivolol is comparable to that of 100 mg atenolol.11
As a further feature, it was shown that Nebivolol does not decrease nocturnal melatonin release 12 which is a common side effect of the 1st and section generation.13 Since a decreased in nocturnal production of melatonin may cause sleep disturbances, a common side effect of beta-blockers of the first and second generation, this finding observed with nebivolol (and carvedilol) might be of practical importance in order to avoid this adverse effect.
In addition, plasma concentrations of Nebivolol do not increase during exercise,14 thus indicating that nebivolol is not taken up into, stored in and released from adrenergic cells during exercise together with noradrenaline, a common feature of most other beta-blockers so far investigated15, which might explain why these beta-blockers may still be effective after withdrawal of therapy even when they are no longer detectable in plasma.
2) Carvedilol
is a non-specific antagonist of adrenergic beta1- and beta2-receptors with additional blocking effects on adrenergic alpha1-receptors.16 Thus, this drug exerts an additional effect independent of beta-blockade that, on the one hand, increases its blood pressure lowering effect and, on the other hand, may decrease potential side effects resulting from beta-blockade since the decrease of blood pressure caused by alpha-blockade may cause a reflectory increase of sympathetic tone, thus reducing beta-blocking (side) effects such as bradycardia, bronchial constriction, impotence, and metabolic side effects.
Furthermore, carvedilol does not reduce nocturnal melatonin release,13 a finding unique to carvedilol and nebivolol among all beta-blockers so far investigated on this issue.12
In addition, plasma concentrations of carvedilol do not increase during exercise,17,18 thus one more finding unique to carvedilol and nebivolol among all beta-blockers so far investigated.
Carvedilol shows an additional feature, namely an increase in heart rate in healthy subjects with the administration of increasing doses of the drug, thus being a unique finding in the class of beta-blockers that increasing doses may cause increasing heart rates (Figure).19,20
3) Sotalol
Sotalol is a non-selective, hydrophilic beta-blocker that prolongs cardiac repolarisation independent of its antiadrenergic action, thus representing class III antiarrhythmic effects.21
Just like all other beta-blockers currently used in cardiovascular medicine, sotalol is a racemic mixture consisting of equal amounts of d-sotalol and l-sotalol, with the d-enantiomer showing solely antiarrhythmic class III effects and the l-enantiomer exerting both antiarrhythmic class III and beta-blocking effects.22.23 Thus, racemic sotalol is a combined beta-blocker and antiarrhythmic class III agent that
- may be useful in the treatment of both ventricular and supraventricular arrhythmias.21,24
The importance of this finding has been emphasised in the SWORD study25 that was terminated prematurely because d-sotalol – the optically pure d-enantiomer that only exerts antiarrhythmic class III effects but no beta-blockade – increased all-cause mortality compared to placebo by 65 % (p = 0.006), mainly due to arrhythmic deaths. Thus, antiarrhythmic class III properties may be useful in order to provide the antiarrhythmic effects of sotalol. However, beta-blockade (effected exclusively by the l-enantiomer) appears to play a major role in the efficacy and safety of sotalol.
4) Propranolol
Propranolol is a non-selective, lipophilic beta-blocker with two additional features: On the one hand, only the non-beta-blocking d-enantiomer inhibits the conversion of thyroxin to triiodothyronin, whereas only the l-enantiomer shows beta-blocking effects.23, 28 Thus, a major part of the efficacy of propranolol in patients suffering from hyperthyroidism resides exclusively in the non-beta-blocking d-enantiomer. This effect on thyroid hormones is well achieved with generally recommended doses of propranolol in humans.
On the other hand, propranolol has been shown to exert antiarrhythmic class I effects residing equally in both the d- and l-enantiomers.28 However, only slight antiarrhythmic class I effects can be achieved in humans even with the highest recommended doses of propranolol in humans. Thus, the clinical relevance of its antiarrhythmic class I effect is questionnable.
Conclusions:
Beta-blockers are not “all equal members of one family of drugs.” On the contrary, there are three different generations of beta-blockers, and some of the drugs exert additional properties independent of beta-receptors, e.g.,
- carvedilol causes vasodilation via inhibition of sympathetic alpha-receptors,
- nebivolol causes NO-derived vasodilation,
- sotalol shows antiarrhythmic class III effects,
- propranolol inhibits the conversion of thyroxine to triiodothyronine.
As a special feature, most beta-blockers, except carvedilol and nebivolol
- are taken up into, stored in and released from adrenergic cells together with noradrenaline. Consequently, their plasma concentrations increase during exercise together with those of noradrenaline and decrease during recovery.
- inhibit the nocturnal production and release of melatonin.
Taken together, some beta-blockers exert further interesting features in addition to their well-known effects on beta-adrenoceptors.
Therefore, beta-blockers should be recognised as individual substances with their own qualities and used according to the individual features, needs and demands of every single patient.
Figure: Heart rates (beats/min) obtained at rest at 3 hours following oral intake of increasing single doses of carvedilol (25, 50, 100 mg), metoprolol
(50, 100, 200 mg) and bisoprolol (2.5, 5, 10 mg): Increasing doses of metoprolol and bisoprolol caused further decreases in heart rate (as expected with beta-blockers), whereas increasing doses of carvedilol caused increases in heart rate, with 200 mg metoprolol and 10 mg bisoprolol being significantly more effective than 100 mg carvedilol; *, p < 0.05 (compared to placebo)
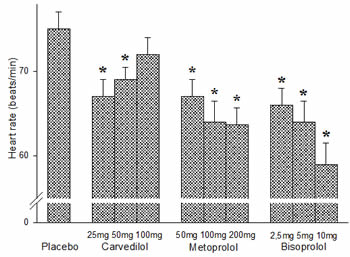
Table 1: The three generations of beta-blockers
1st generation
- non-selective e.g., propranolol, sotalol
- particularly indicated in:
- portal hypertension and hyperthyrosis (propranolol)
- special arrhythmias (sotalol)
2nd generation
- beta1-selective "cardioselective"
e.g., metoprolol, bisoprolol - particularly indicated in:
- coronary artery disease,
- tachyarrhythmias, heart failure
3rd generation
- vasodilating e.g. carvedilol, nebivolol
- particularly indicated in:
- arterial hypertension,
- heart failure
Table 2: Additional features of some beta-blockers
- Beta-blocker : Additional feature(s)
- Propranolol : Inhibition of the conversion T4 – T3
- Slight antiarrhythmic class I effect
- Sotalol: Antiarrhythmic class III effect
- Carvedilol : Inhibition of sympathetic alpha1-receptors
- No effect on nocturnal melatonin release
- No release from adrenergic cells
- Nebivolol: High beta1-selectivity
- NO-derived vasodilation
- No effect on nocturnal melatonin release
- No release from adrenergic cells
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.