Atrial flutter seems to be an easy electrocardiographic (ECG) diagnosis, which can be done by a medical student. It is treated in daily practice mostly with DC cardioversion and subsequent antiarrhythmic drug use.
However, only rarely do the doctors actually analyse the circumstances which have brought on the arrhythmia.
Avoiding these triggering circumstances might help in preventing future attacks.
Furthermore, certain patients are referred for radiofrequency ablation (which is an effective treatment of "classical" atrial flutter), when in fact their true diagnosis is left atrial focal tachycardia - where radiofrequency ablation is substantially more difficult and provides only questionable long-term benefit.
Case description
As an introduction, I describe an example, of how atrial tachycardia (clearly triggered by external factors) was falsely diagnosed as flutter.
The 53-year old normotensive male patient with no previous history of cardiac disease and a normal recent coronary CT scan was admitted for sudden onset of palpitations. He was exhausted after overnight work - he had not slept in the last 36 hours and had consumed 7 cups of coffee and 4 glasses of Coka-Cola during this period. The arrhythmia was triggered after having accidentaly swallowed an ice cube while drinking the last glass of Coke.
The palpitations started precisely when the ice was passing through his oesophagus. Within 30 minutes, an ECG was recorded (fig. 1) and a full examination done. Admission blood pressure was 160/110 mmHg, his potassium level was 3,4 mmol/l, his physical examination and echocardiogram normal. The admission diagnosis was atrial flutter. The initial treatment was enoxaparine subcutaneously and propafenon intravenously. The arrhythmia was not altered by propafenon, thus DC cardioversion was planned for the next morning. Treatment was extended with intravenous potassium, magnesium and metoprolol and with oral diazepam.
The patient slept for 6 hours and woke up in the early morning with a sinus rhythm. After re-discussing the ECG and the triggering moment, the arrhythmia was re-diagnosed as probable left atrial focal tachycardia, triggered by the ice passing esophagus during a "fragile period“ (stress + excess caffeine + lack of sleep). Hypokalemia and hypertension were possibly caused by stress and caffeine. The patient stopped caffeine completely, resumed more regular sleeping habits and remained asymptomatic with low blood pressure and without any further therapy.
Epidemiology of atrial flutter
The overall incidence of atrial flutter is 0,09% (1), 58% of patients also have atrial fibrillation in their history. Atrial flutter represents 0,1% of hospital discharges in the US, with the mean age at 67 years and male predominance cca 2:1. Case fatality is 1%, mostly related to underlying disease (1).
Etiology
Any supraventricular arrhythmia can be triggered by one ore more precipitating factors: excessive caffeine intake, alcohol (either from a single excess or regular drinking), nicotin, certain drugs, hyperthyreoidism, stress, menstruation, electrolyte disturbance, hypovolemia, fever, infection or lack of sleep.
- A first occurence of atrial flutter is in 60% of cases associated with a specific acute precipitating event (major surgery, pneumonia, myocardial infarction).
- In 38% of cases, atrial flutter is associated with chronic illness (heart failure, lung disease, hypertension).
- “Lone” atrial flutter (without any recognisable underlying disease) is rare – only 2% of atrial flutter patients (2).
An overview of ethiologic and precipitating factors, which may trigger atrial flutter is in table 1.
Pathophysiology
Atrial flutter is a typical macro-reentrant tachycardia, i.e. the re-entry circuit occupies large areas of the atrium. Most typically, tachycardia rotates in the right atrium counter-clockwise around the tricuspid valve anulus (cavo-tricuspid isthmus – dependent flutter). Atrial rhythm is typically around 300 / min (250-350/min.)
Clinical picture
The most frequent symptoms of atrial flutter are palpitations and/or mild chest dyscomfort. More severe symptoms (dyspnea, pre-syncope) may occur in patients with diminished reserve (e.g. left ventricular dysfunction, respiratory insufficiency etc.). Polyuria is caused by the release of atrial natriuretic peptide in response to increased atrial pressures from contractions of atria against a closed AV valve.
Differential diagnosis
A surface 12-lead electrocardiogram (ECG) is frequently sufficient for diagnosis, but it may be difficult to differentiate atrial flutter from focal atrial tachycardias or other supraventricular tachycardias, which have different mechanisms and treatment.
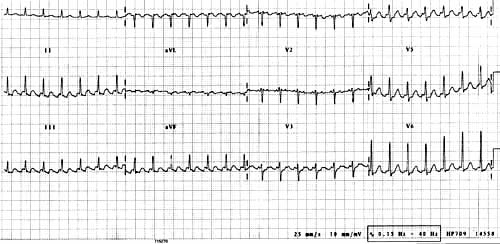
Atrial flutter usually has the atrial rate at almost precisely 300 / min. and ventricular rate most oftentimes at 150 / min. (2:1 A-V block). Vagal stimulation, adenosine or betablockers may increase the degree of A-V block and classical "flutter waves" can be visualised on the ECG as positive atrial waves in V1 and negative "sawtooth" pattern atrial waves in III, aVF (fig. 2).
ECGs should always be read by an experienced physician – automated analysis systems of 12-lead ECG are unreliable and commonly suggest incorrect arrhythmia diagnosis (1).
Transesophageal ECG recordings of the atrial activity may be useful to distinguish flutter from some other arrhythmias. Invasive electrophysiological examination (intracardiac ECG) is indicated usually only when connected with treatment (see below). Differential diagnosis of atrial flutter and other arrhythmias is in table 2.
Non-pharmacologic treatment
DC-synchronized shock (50 J) is indicated in all urgent situations (e.g. hemodynamic compromise). The success rate is between 95-100%. Alternative non-pharmacologic treatment by atrial overdrive pacing (transvenous or transoesophageal) has a success rate of 82% and is especially used during the post-operative period in cardiac surgery. The recently published LADIP trial (3) showed a 100% success rate of radiofrequency ablation as first line treatment.
Antiarrhythmic drugs for conversion to sinus rhythm
Intravenous betablockers or calcium channel blockers (dilitiazem or verapamil) slow the heart rate, but in few patients can it terminate the arrhythmia. Intravenous ibutilide converts atrial flutter to sinus rhythm in 38-76% and this occurs within cca 30 minutes (4). However, the incidence of sustained or nun-sustained ventricular tachycardia after ibutilide was up to 7%. Similar effectivity can be achieved with dofetilide. Other antiarrhythmic drugs are not significantly better than placebo: intravenous propafenone converts only 40% of atrial flutter patients, sotalol 30% and flecainide only 13%. Amiodaron is also not effective for the conversion of this arrhythmia.
Antiarrhythmic drugs for prevention of atrial flutter recurrence
Oral dofetilide has 73% efficacy for the maintenance of sinus rhythm at 1 year, while oral flecainide has 50% long-term efficacy. The experience with any oral drugs in this setting is very limited as most trials combined atrial fibrillation patients with atrial flutter patients and the former group dominated the trials. Oral betablockers or calcium channel blockers can be used effectively to slow the heart rate in cases of recurrence. Their true value for the prevention of atrial flutter recurrence was not tested in a randomised trial.
Anticoagulant therapy in atrial flutter
The risk of embolisation during cardioversion for atrial flutter ranges between 1,7 – 7,0%, the mean was 2,2% (1). The incidence of atrial echo-dense material or clot varies between 0 – 34% in patients with atrial flutter without anticoagulation therapy and occurs usually with > 48 hours duration of the arrhythmia. Furthermore, atrial stunning (absence of atrial contractions) was described several weeks after cardioversion in some patients. Thus, the guidelines for anticoagulation in atrial flutter should be the same as for atrial fibrillation. Cardioversion should be done only with adequate anticoagulation, or within < 48 hours after the arrhythmia onset or when transoesophageal echocardiography shows no atrial clots. Recurrent atrial flutter or even the first episode in high-risk patients with structural heart disease is indicated for long-term oral anticoagulation.
A summary of therapeutic approches is in table 3.
Table 1 : Ethiologic and precipitating factors, which may trigger atrial flutter
| FACTORS WHICH MAY TRIGGER "LONE" ATRIAL FLUTTER (IN THE ABSENCE OF ANY OTHER DISEASE) | DISEASES WHICH MAY BE ACCOMPANIED/COMPLICATED BY ATRIAL FLUTTER |
| Nicotine | Pulmonary diseases (acute or chronic) |
| Alcohol | Cardiac / pulmonary surgery (postoperative) |
| Caffeine | Acute myocardial infarction |
| Stress or anxiety | Heart failure |
| Hypokalemia | Hypertension |
| Drugs | Congenital heart disease |
| Acute infection | Valvular heart disease |
| Lack of sleep |
Table 2 : Differential diagnosis of atrial flutter and other arrhythmias
| NARROW QRS-COMPLEX TACHYCARDIAS | WIDE QRS-COMPLEX TACHYCARDIAS | FOCAL ATRIAL TACHYCARDIAS | ATRIAL FLUTTER |
| ECG during carotid massage or iv. adenosine injection slows the ventricular rate and demasks atrial waves | SVT with BBB: most BBB’s are not rate-related, but BBB ("aberration") may occur with any tachycardia | Isoelectric baseline is present between P waves | "Sawtooth" pattern (isoelectric baseline is not present between P waves) |
| Esophageal ECG electrodes (when surface ECG is not diagnostic) | Accessory pathway: "delta" waves in preexcitation syndromes, LBBB-type QRS complex in some types of accessory pathways |
Atrial rates most frequently 200 – 260 / min., rarely 300 / min. | Dominant negative "flutter" waves in III, aVF + positive "flutter waves in V1 in typical "counterclockwise" isthmus-dependent flutter or vice-versa in rare "clockwise" isthmus-dependent flutter |
| No P waves visible – AVNRT most likely | Ventricular tachycardia: A-V dissociation (ventricular rate is faster than atrial rate), QRS > 0,16 s (with LBBB morphology or > 0,14 s (with RBBB morphology), RS interval > 100 ms in any precordial lead (initial R – nadir S), QS-type complexes in all precordial leads |
Right atrial origin: Positive or biphasic P waves in aVL + negative or biphasic P waves in V1 | Atrial rate typically around 300 / min. (range 250-350), ventricular rate most typically 150 / min. (A-B block 2:1) |
| P waves in ST segment and no A-V block – AVRT most likely | Left atrial origin: negative P waves in I, aVL + positive P waves in V1 | ||
| P waves obscured by the T waves of the preceeding complex | |||
| Presence of A-V block excludes AVRT or AVNRT | |||
| This diagnosis can be established with absolute certainity only by an electrophysiologic study |
Table 3 : Overview of treatment approaches to atrial flutter and similar arrhythmias
| NON-PHARMACOLOGIC TREATMENT | DRUGS FOR CONVERSION TO SINUS RHYTHM | DRUGS FOR PREVENTION OF RECURRENCE | ANTICOAGULANT DRUGS |
| DC-synchronised shock (50 J) is the most effective acute treatment | Less effective than non-pharmacologic treatment | None has proven effect | Same recommendation as for Atrial Fibrillation |
|
Atrial overdrive pacing (transvenous or transoesophageal) |
Ibutilide | Dofetilide? | Anticoagulation therapy is indicated for all patients with atrial flutter except those with contraindication and except patients with "lone" atrial flutter |
| Radiofrequency ablation (as the first line treatment or as prevention of recurrence) | Dofetilide | Flecainide? | |
| Betablockers? | |||
| Calcium channel blockers? |
Fig. 1: Left atrial focal tachycardia
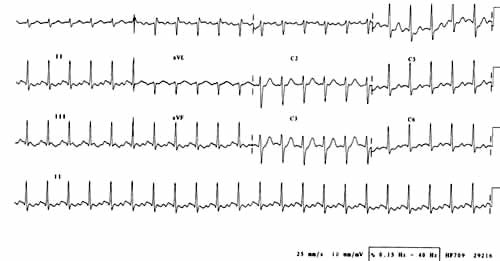
Fig. 2: Atrial flutter
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.