The New European Society of Hypertension/European Society of Cardiology (ESH/ESC) Guidelines on hypertension, issued in 2007, offer an in-depth examination into the problem of blood pressure control during treatment, emphasising the need in current clinical practice for combination drug treatment. Guidelines address in this regard a number of clinically relevant questions, such as:
- which are the requirements for a combination drug treatment
- when is combination drug treatment needed?
- are fixed combinations preferable to extemporaneous ones?
- which combinations of priority use?
On these questions (and on the related answers) is focused the present article
Combination treatment allows hypertensives to achieve hypertension levels closer to ones of untreated individuals.
A large number of controlled studies have conclusively shown that treatment of hypertension is beneficial. In virtually all hypertensive conditions, drugs that lower diastolic and/or systolic blood pressure reduce cardiovascular morbidity and mortality (1, 2).
However, this is counterbalanced by the evidence that current management of hypertension is unable to bring the cardiovascular risk of the treated hypertensive patients back to the level of the normotensive individuals (3).
Although several factors are believed to be responsible for this finding, a likely candidate is poor blood pressure control, i.e. the fact that blood pressure levels of treated hypertensives remain, almost invariably, higher than those of normotensive controls. This limitation can be overcome by a therapeutic strategy based on a combination of two or more antihypertensive drugs, which allows to achieve a better blood pressure control (and thus greater cardiovascular protection) in a much larger fraction of hypertensive patients (4). This is one of the reason for which this therapeutic approach has been recommended by the 2007 European Society of Hypertension/European Society of Cardiology Hypertension Guidelines (5).
I - RATIONALE AND REQUIREMENTS
Combination therapy is successive overall and has five main requirements
Whereas initial monotherapy effectively lowers blood pressure in only a limited fraction of the hypertensive population, combined administration of two or three drugs achieves a successful antihypertensive response in about 80% and 90% of cases, respectively. Combination therapy plays a fundamental role in the overall treatment of hypertension that is not limited to clinical practice (and thus to the possible incorrect use of single-drug regimens) ; combination treatment with two and three drugs has also been commonly employed to achieve optimal blood pressure in controlled studies. Optimal two-drug combinations are characterised by five main requirements.
- First, the drug to be combined should display mechanisms of action that are different but complementary.
- Second, they should, when given together, produce an antihypertensive effect that is greater than, or equal to, the sum of the antihypertensive effect of the individual combination components, although an effect that is just greater than that of either drug alone may also be acceptable.
- Third, there should also be total or partial summation of their ability to protect against the organs that are damaged by hypertension, e.g. they should produce a regression of left ventricular hypertrophy or a reduction in proteinuria greater than what can be achieved with the individual combination components.
- Fourth, they should reciprocally reduce (or at least not increase) their side effects.
- Fifth, they should not have untoward (adverse) haemodynamic and humoral effects.
II - FIXED VERSUS EXTEMPORANEOUS COMBINATIONS
Extemporaneous combinations are flexible and increase physician awareness
Fixed combinations have advantages, but also disadvantages, over the separate administration of the same drugs. Extemporaneous combinations :
- obviously allow flexible dosing of the components, e.g. the dose of one drug may be increased while keeping the other constant, if this is felt to be useful.
- facilitate a greater awareness, by the physician, of the constituents of the combination treatment, thus reducing the risk of administering contraindicated drugs and allowing better identification of which drug is responsible for the side effects that may appear during treatment (6).
Except for the flexibility of dosing, these advantages, however, are not in principle incompatible with fixed-dose combinations, provided that doctors receive proper information.
Fixed combinations help with patient compliance and reduce the cost of treatment.
However, fixed combinations have specific advantages. It should be remembered that fixed combinations allow blood pressure control to be achieved with a reduced number of daily tablets compared with extemporaneous combinations, thus simplifying the therapeutic approach.
- This is of great potential advantage because blood pressure control in the hypertensive population is unsatisfactory, i.e. in only a minority of the hypertensive population is diastolic blood pressure reduced by antihypertensive treatment to 90 mmHg or less (7-8). This is even more evident for systolic blood pressure which is only controlled in a minority of hypertensive individuals, with no trend towards any improvement in the last few years (9). This is due largely to poor compliance with long-term treatment due to a number of factors, among which the complexity of the treatment scheduled.
- Other favourable features of fixed combination are represented by the reduced treatment cost as compared to the cost of using the same drugs on a separated basis, with further advantages for compliance. This has been acknowledged by the ESH/ESC 2007 Guidelines of hypertension (5), which mention fixed combinations as an asset for antihypertensive treatment and a further means to improve blood pressure control in the hypertensive population.
III - WHEN TO START
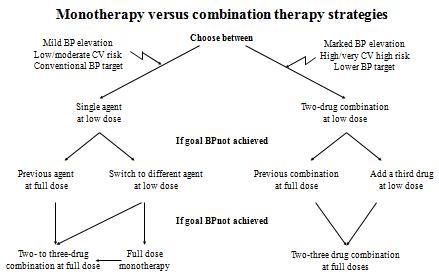
ESH/ESC 2007 Guidelines (5) make a clear statement on the use of monotherapy and combination drug therapy strategies (Figure). They first emphasise that combination treatment “is needed to control blood pressure in the majority of patients”, making the issue related to the drug of first therapeutic choice less relevant.
They also recognise that combination treatment is almost mandatory in diabetic, renal and high risk hypertensive patients because in all these clinical conditions blood pressure goal is set at 130/80 mmHg or even lower and thus a large blood pressure reduction is oftentimes needed, making the use of single monotherapy not recommended.
Guidelines make a further point in favour of combination therapy, underling the concept that starting treatment with a two-drug combination may allow blood pressure targets to be reduced earlier than with monotherapy. This is of particular importance in high-risk patients, in the light of the evidence provided by the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) study that a lack of a prompt blood pressure control may be associated in these individuals with a higher events rate (10)
IV - COMBINATION OF PRIORITY USE
According to 2007 ESH/ESC Guidelines (5) combination of priority use includes the following:
- Thiazide diuretic and ACE inhibitor
- Thiazide diuretic and angiotensin receptor antagonist
- Calcium antagonist and ACE inhibitor
- Calcium antagonist and angiotensin receptor antagonist
- Calcium antagonist and thiazide diuretic
- Beta-blocker and calcium antagonist (dihydropiridine)
In practical terms the choice of the preferable combination of drugs regimen should be based on a number of factors, including the patient’s age, metabolic and cardiovascular risk profile, the presence of target organ damage, tolerability and side effects of the combinations used.
A final recommendation given by the ESH/ESC 2007 Guidelines refers to the use of low-dose combinations. These should be preferred to high dose combinations because they
- frequently allow to achieve to an antihypertensive efficacy greater for magnitude than that obtained by high doses and
- display a much better tolerance profile, which is of key importance for patients compliance to treatment and thus for the clinical success of antihypertensive therapy.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.