Hypertrophic cardiomyopathy (HCM) is a relatively common form of heart disease due to genetic disorders and it is the most frequent cause of sudden death in young individuals (1-2). The clinical phenotype is extremely variable and although the distribution of left ventricular hypertrophy has shown little relation to clinical outcome, the magnitude of left ventricular wall thickness conveys prognostic significance (2). Two dimensional echocardiography is the standard imaging technique for the diagnosis, however this modality can fail to identify hypertrophy in a number of patients due to technical reasons. Cardiac Magnetic Resonance Imaging is an alternative approach which offers tissue contrast and a border definition that are often superior to what is achievable with echocardiography (3).
The regions in which 2-D Echocardiography led to a tendency to underestimate the degree of hypertrophy are the antero-lateral wall (4) and the apical region (5). It is noteworthy to underline that in some cases MRI has made it possible to detect an extreme degree of hypertrophy ( 28 mm) in the presence of an inconclusive echocardiographic examination, leading to a significant change in the prognostic stratification of these patients - with some of them moved to the group of higher risk for sudden cardiac death and implying a more aggressive therapy such as the positioning of an implantable defibrillator. It is also remarkable that this tendency to underestimate the presence of hypertrophy shown by Echocardiography does not seem to be related to the inadequate level of the equipment used in these studies, which on the contrary can be considered as state of the art at the time of publication. In fact, this result seems rather to be related to the geometrical limitation intrinsic to the transthoracic approach.
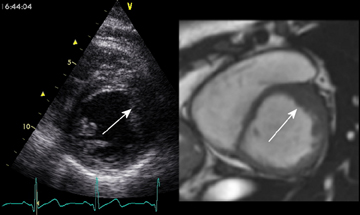
In Figure 1 and 2 a case of hypertrophic cardiomyopathy. In this patient the familiar history was negative, the ECG was doubtful (Figure 1), the echocardiogram resulted inconclusive due to an inadequate acustic window (Figure 2, left panel) and the MRI findings led to the final diagnosis (Figure 2, right panel).
Figure 1
ECG findings in a patient with HCM. The lack of R waves in V1-V4 are “per se” non specific.
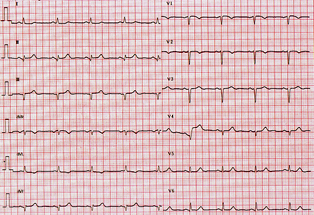
Figure 2
Same case of Figure 1. Left panel: echocardiographic short axis of left ventricle. The drop out of the signal at the level of the antero-lateral wall (arrow) makes the echocardiogram inconclusive.
Right panel: the MR image allows an easy depiction of morphology in all cardiac segments and the detection of anterolateral hypertrophy (arrow).
These findings confirm the idea that hypertrophic cardiomyopathy has been consistently underestimated and raise the problem of the integrated and proper use of these imaging modalities. It seems reasonable to propose two dimensional echocardiography as the first line imaging technique and standard approach for the diagnosis as it is much more feasible than cardiac MRI which still has some limited availability. On the other hand, a further effort in the diagnostic pathway should not be omitted when a patient has unexplained ECG findings that are compatible with regional hypertrophy or whenever familiar history, genetic findings or the clinical history are such that a significant probability of the disease is existing also in presence of an inconclusive echocardiogram.
The content of this article reflects the personal opinion of the author/s and is not necessarily the official position of the European Society of Cardiology.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.