Introduction
Cardiovascular disease (CVD), of which coronary heart disease (CHD) is the most common, is the leading cause of death in Europe. Despite recent decreases in mortality rates in many countries, CVD is responsible for over four million deaths per year, nearly half of all deaths in Europe. The proportion of all deaths attributable to CVD is greater among women (51%) than men (42%) and the burden of mortality continues to show large geographic inequalities. Coronary heart disease (CHD) accounts for almost 1.8 million deaths, or 20% of all deaths in Europe annually [1].
The main objectives of cardiovascular disease prevention are to reduce morbidity and mortality and increase the chances of a longer life expectancy [2-6]. There is a wealth of scientific evidence from observational studies and randomised controlled trials demonstrating that lifestyle intervention in relation to smoking, diet and exercise, treatment of hypertension, hyperlipidaemia, and diabetes, and the use of prophylactic drug therapies can reduce morbidity and mortality and improve quality of life in people with coronary disease.
The European Society of Cardiology together with other partner societies has engaged in a comprehensive programme of CVD prevention in clinical practice since 1992. The Joint European Societies’ (JES) guidelines on the prevention of CVD in clinical practice published in 1994, 1998, 2003, 2007 and 2012 [2-6] gave the highest priority to patients with coronary or other atherosclerotic disease. The aim of the JES guidelines on CVD prevention is to improve the practice of preventive cardiology by encouraging the development of national guidance on cardiovascular disease prevention and its communication, implementation and evaluation through the national societies in each country. The 2012 JES guidelines defined the lifestyle and risk factor targets for patients with CHD as follows: stop smoking, make healthy food choices and be physically active; a body mass index (BMI) less than 25 kg/m²; blood pressure <140/90 mmHg (<140/80 mmHg in patients with diabetes mellitus); low-density lipoprotein (LDL) cholesterol less than 1.8 mmol/L (<70 mg/dL) or at least 50% reduction, glycated haemoglobin (HbA1c) <7.0 mmol/L (<53 mmol/mol in people with diabetes mellitus) and appropriate use of cardioprotective drug therapies, in addition to medication used for the treatment of elevated blood pressure, lipids and glucose: aspirin or other platelet-active drugs, beta-blockers, angiotensin-converting enzyme (ACE) inhibitors/angiotensin II receptor blockers (ARBs) and antithrombotic drugs [6].
EUROASPIRE surveys
Background
Audits of clinical practice provide an objective assessment of clinical outcomes and quantify the extent to which the standards set in the guidelines on CVD prevention are being implemented in everyday clinical practice. However, risk factor management in patients with CHD in Europe is far from optimal. Implementation of the JES guidelines in Europe was evaluated in four cross- sectional surveys called EUROASPIRE (European Action on Secondary and Primary Prevention by Intervention to Reduce Events). EUROASPIRE I was conducted in 1995-96 in nine countries under the auspices of the Working Group on Epidemiology and Prevention and was followed by a second and a third survey in 1999-2000 (15 countries), and in 2006-2008 (22 countries) through the Euro Heart Survey programme. The most recent EUROASPIRE IV survey was carried out in 2012-2014 (24 countries) under the auspices of the European Society of Cardiology, EURObservational Research Programme [7-15]. The main objectives of each survey were to identify risk factors in patients with CHD, describe their management through lifestyle and the use of cardioprotective drug therapies, and to provide an objective assessment of clinical implementation of current scientific knowledge. The fourth EUROASPIRE survey merged with the Euro Heart Survey on Diabetes [16] and created the first European Survey on Cardiovascular Disease Prevention and Diabetes, incorporating an assessment of dysglycaemia (impaired fasting glycaemia, impaired glucose tolerance and new diabetes) in all patients.
EUROASPIRE IV survey
EUROASPIRE IV was carried out in 24 European countries: Belgium, Bosnia & Herzegovina, Bulgaria, Croatia, Cyprus, Czech Republic, Finland, France, Germany, Greece, Ireland, Latvia, Lithuania, The Netherlands, Poland, Romania, Russia, Serbia, Slovenia, Spain, Sweden, Turkey, Ukraine and the UK. Within each country one or more geographical areas with a defined population were selected and a sample of one or more hospitals was taken so that any patient presenting within the area with acute symptoms of coronary disease, or requiring revascularisation in the form of balloon angioplasty (PCI) or coronary artery surgery (CABG), had an approximately equal chance of being included. A total of 7,998 coronary patients were interviewed at least six months after admission for an acute coronary event or procedure. The median time between index event and interview was 1.35 years (IR 0.95-1.93 years) [11, 12].
Consecutive patients, men and women (≥18 years and <80 years of age at the time of their index event or procedure), with the following first or recurrent clinical diagnoses or treatments for CHD were retrospectively identified from diagnostic registers, hospital discharge lists or other sources: (i) elective or emergency CABG, (ii) elective or emergency PCI, (iii) acute myocardial infarction, and (iv) unstable angina. The methodology used in EUROASPIRE I was replicated in the second, third and fourth surveys with standardised interviews and measurements, and a central laboratory for lipid and glucose analyses, so that time trends between surveys could be described.
The EUROASPIRE IV results showed that a large majority of coronary patients in Europe did not achieve the guideline standards for secondary prevention set by the 2012 JES guidelines on CVD prevention in clinical practice, with a high prevalence of persistent smoking, unhealthy diets, and physical inactivity. Consequently, most patients were overweight or obese with a high prevalence of diabetes [11-13] (Figure 1). There was considerable variation between European countries in patients’ lifestyle, risk factor prevalence and the use of cardioprotective medication. Information on risk factor history and measurements in the discharge documents was incomplete. At discharge, smoking status and obesity were recorded in about two thirds of patients and in one fifth of patients there was no information recorded on blood pressure, lipids or glucose metabolism.
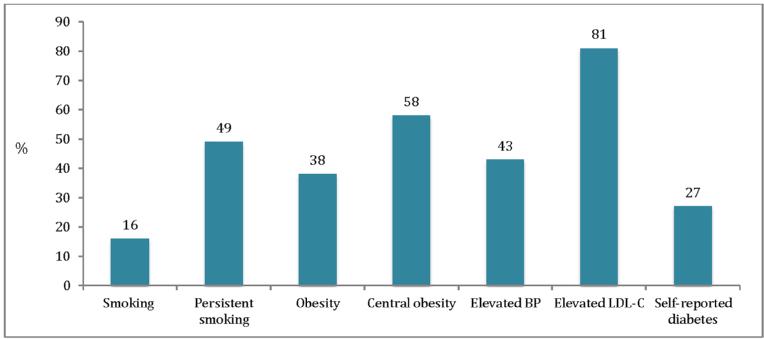
Figure 1. EUROASPIRE IV: prevalence of smoking, persistent smoking, obesity, central obesity, elevated blood pressure and LDL-cholesterol, and self-reported diabetes.
Smoking: self-reported smoking or >10 ppm carbon monoxide in breath; Persistent smoking: self-reported smoking or >10 ppm carbon monoxide in breath in patients reporting to have been smoking in the month prior to the index event; Obesity: BMI ≥30 kg/m²; Central obesity: waist circumference ≥88 cm for women and ≥102 cm for men BP: ≥140/90 mmHg (≥140/80 mmHg in patients with diabetes mellitus); LDL-C: ≥1.8 mmol/L
Cardiac rehabilitation is an effective treatment for patients with CHD, reducing both cardiac and total mortality [17]. There is strong scientific evidence that lifestyle modifications in relation to tobacco smoking, diet and physical activity can reduce the risk of recurrent cardiovascular events in patients with established CHD and can improve survival. It is a major cause for concern that nearly three fifths of patients in EUROSPIRE IV reported little or no physical activity and were centrally obese and two fifths were obese. A meta-analysis of smoking cessation after a myocardial infarction showed a relative risk reduction of coronary mortality by 46% in those who stopped smoking compared with those who continued to smoke [18]. In EUROASPIRE IV, the prevalence of current smoking was 16% and it was highest in patients <50 years old in both men and women. Nearly half of patients who were smokers in the month prior to a coronary event were still smoking at the time of interview. It is worrying that only about half of patients reported having the intention to quit smoking and only a small minority attended a smoking cessation clinic or used pharmacotherapy to try to stop smoking.
Following myocardial infarction, elevated blood pressure is associated with an increased risk of reinfarction, coronary death or stroke. All coronary patients require specific lifestyle advice and, where appropriate, antihypertensive medication. The meta-analysis of randomised trials of blood pressure-lowering medication in patients with coronary disease showed that a reduction of systolic blood pressure by 10 mmHg or diastolic blood pressure by 5 mmHg reduces fatal and non-fatal CHD events by about one quarter and stroke by about one third [19]. However, the control of blood pressure in EUROASPIRE IV was far from optimal with more than two fifths of patients not reaching the blood pressure goal.
Large-scale clinical trials and meta-analyses have demonstrated that cholesterol-lowering therapies, especially statins, reduce recurrent cardiovascular events and can prolong survival in patients with established CVD. A prospective meta-analysis of data from 90,056 individuals in 14 randomised trials showed that statin therapy can safely reduce the five-year incidence of major coronary events, coronary revascularisation, and stroke by about one fifth per mmol/L reduction in LDL cholesterol, largely irrespective of the initial lipid profile or other presenting characteristics [20]. Recent trials addressing more aggressive lipid-lowering therapy confirmed that lowering LDL cholesterol to ≤1.8 mmol/L (<70 mg/dL) is associated with the lowest risk of recurrent CVD events in patients with established CVD [21]. Therefore, in the 2012 JES5 guidelines, the recommended target for LDL cholesterol was reduced to <1.8 mmol/L or at least a 50% reduction from baseline LDL cholesterol. Overall, four fifths of patients in EUROASPIRE IV had LDL cholesterol ≥1.8 mmol/L (>70 mg/dL) and only one fifth of those on lipid-lowering medication achieved the LDL cholesterol goal.
The risk of dying for patients with coronary artery disease and diabetes is substantially higher than for those free from diabetes [22]. Self-reported diabetes was found in one quarter of coronary patients. Glucose control was poor with just over half reaching the HbA1c target of <7 mmol/L (53 mmol/mol). A multifactorial intervention directed towards lifestyle, risk factor control and use of evidence-based medications is recommended to reduce microvascular and to a lesser degree macrovascular complications in patients with type 2 diabetes mellitus.
The following cardioprotective drug therapies have been shown to reduce morbidity and mortality in clinical trials and are recommended in the JES5 guidelines for CVD prevention: aspirin or other platelet-modifying drugs in all patients, beta-blockers in those after myocardial infarction, ACE inhibitors/ARBs in those with impaired left ventricular function, and statins in all patients. A large majority of EUROASPIRE patients reported taking these medications. Antiplatelets were prescribed in 94%, beta-blockers in 83%, ACE inhibitors/ARBs in 75%, and statins in 86%. The possible explanation of inadequate blood pressure and lipid control, despite the high use of these medications, is that treatment is initiated with low-dose prescriptions, and then not titrated up, as well as poor patient adherence, or both. Therefore, many patients will require more intensive blood pressure and cholesterol management and optimal use of cardioprotective medications to achieve their targets.
Time trends in risk factor management between 1999 and 2013
A comparison across the most recent three surveys provided a unique description of time trends for secondary prevention in the same countries, geographical areas and hospitals over a period of 14 years [14, 15]. The results demonstrated adverse lifestyle trends, a significant increase in obesity, central obesity and diabetes, and a high prevalence of persistent smoking among younger patients and especially women. The prevalence of smoking was virtually unchanged over the three surveys with about one in five patients still smoking at the time of interview. The prevalence of obesity and central obesity increased significantly by 7% and 6%, respectively. These adverse trends in body weight and distribution most probably contribute to the poor control of other risk factors such as raised blood pressure, dyslipidaemia and diabetes.
Although blood pressure and lipid management improved, these risk factors were still not optimally controlled. The proportions of patients with raised blood pressure and elevated LDL cholesterol decreased significantly by 9%, and by 21%, respectively. However, many patients on antihypertensive and lipid-lowering medication had not reached the blood pressure and LDL cholesterol goal. The rising prevalence of obesity and central obesity was probably contributing to the rising prevalence of diabetes, showing an absolute increase of about 8% across the surveys. The glucose control in patients with self-reported diabetes remained unchanged across the three surveys with only a minority of patients achieving the target of fasting glucose <7.0 mmol/L. Although the frequency of cardioprotective drug use had increased substantially between the EUROASPIRE II and EUROASPIRE III surveys, no further significant change was observed between the third and fourth surveys. However, there was a twofold increase in the proportion of patients on high-intensity statins between the EUROASPIRE III and IV surveys.
Lessons for clinicians
The EUROASPIRE surveys give a unique picture of preventive cardiology in Europe as practised by cardiologists, primary care physicians and other healthcare specialists looking after patients with coronary disease. EUROASPIRE IV continues to show that implementation of JES guidelines on secondary prevention is far from optimal. A large majority of coronary patients do not achieve the lifestyle and medical risk factor targets. Adverse trends in smoking prevalence and the alarming increase in obesity, central obesity and diabetes are an increasing cause for concern. Although most patients are prescribed cardioprotective drugs, blood pressure, lipid and glycaemic control is still inadequate and there are large variations in secondary prevention practice between countries.
Practitioners need clear and practical guidance, applicable to the patients seen in their practice, and in accordance with national, cultural, and socioeconomic aspects of their countries. Optimal control of CVD risk factors is one of the most effective methods for reducing vascular events in patients with CHD. All cigarette smokers should be professionally encouraged and offered pharmacological support to stop smoking. Coronary patients should receive professional advice on healthy diet and how to increase their physical activity. The risk of recurrent disease can be further reduced by optimising the prescription of cardioprotective medication, combining different drugs and up-titrating them to the doses showing efficacy and safety in randomised controlled clinical trials. Improving treatment adherence is a very important step in optimising cardiovascular risk factor management. In clinical practice, physicians should always assess treatment adherence and identify reasons for non-adherence.
Conclusions
Preventive cardiology needs a systematic, comprehensive, multidisciplinary approach, which addresses lifestyle and risk factor management by cardiologists, other specialists, general practitioners, nurses and other allied health professionals, and a healthcare system which invests in prevention. Saving people’s lives from acute heart attacks is not sufficient and coronary interventions should always be followed by prevention. All coronary patients require a modern preventive cardiology programme, combining a professional lifestyle intervention with effective risk factor management to achieve better risk factor control and reduce the risk of recurrent cardiovascular events.
Acknowledgements
EUROASPIRE surveys were carried out under the auspices of the European Society of Cardiology, Euro Heart Survey and subsequently the EURObservational Research Programme through unrestricted research grants from Merck, Sharp & Dohme (EUROASPIRE I), AstraZeneca, Bristol-Myers Squibb, Merck, Sharp & Dohme and Pfizer (EUROASPIRE II); AstraZeneca, Bristol-Myers Squibb, GlaxoSmithKline, Merck/Schering-Plough, Novartis, Pfizer, Sanofi-Aventis, Servier (EUROASPIRE III); and Amgen, AstraZeneca, Bristol-Myers Squibb and AstraZeneca, F. Hoffman-La Roche, GlaxoSmithKline, and Merck Sharp & Dohme (EUROASPIRE IV). The sponsors of the EUROASPIRE surveys had no role in the design, data collection, data analysis, data interpretation, decision to publish, or writing the manuscript.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.