Background
Over the past decades, catheter ablation has increasingly been recognised as an effective method for the treatment of diverse types of cardiac arrhythmias. Introduction, development and our growing experience with three dimensional mapping systems have improved both the safety and efficacy of this invasive therapy. In the following paragraphs, the indications and basic principles of ablation of supraventricular tachycardias (excluding atrial fibrillation) will be presented mainly from the perspective of a non-electrophysiologist, within the context of the latest ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias.
1- Isthmus-dependent flutter
A) Presentation
Isthmus dependent flutter is a tachycardia attributed to a macroreentrant circuit located in the right atrium, with a rate usually ranging from 250 to 350 beats per minute. In the most frequent type, (counterclockwise type - 90% of cases), the waveform propagates in a craniocaudal direction along the free wall of the right atrium and in a caudocranial direction along the interatrial septum. The reverse direction is followed in cases of the more rarely encountered reverse typical flutter. The site of interest, both from a pathophysiologic perspective (area of slow conduction contributing to the perpetuation of the macroreentrant circuit) as well as from a therapeutic perspective (target area during ablation) is the cavotricuspid isthmus. The cavotricuspid isthmus is a portion of the inferior right atrium, demarcated anteriorly by the tricuspid valve annulus and posteriorly by the inferior vena cava as well as by the eustachian ridge.
B) Technique
During flutter ablation, a linear lesion is deployed along the cavotricuspid isthmus extending from the tricuspid valve to the ostium of the inferior vena cava (Figure 1) (1). Primary aim is the deployment of the line along the central part of the isthmus (6 o’clock in left anterior oblique projection), due to the shorter pathlength and the reduced width of the cavotricuspid isthmus in this particular area. It should be pointed out that procedural endpoint during isthmus ablation is not only termination of the tachycardia, but also the documentation of bidirectional block along the linear lesion using electrophysiological maneuvers.
Catheter ablation is highly effective in both the termination of isthmus-dependent flutter as well as in the prevention of future recurrences. It is significantly more effective than antiarrhythmic agents in preventing recurrences of isthmus dependent atrial flutter and in reducing arrhythmia-related hospitalisations. In a post-catheter ablation one-year follow-up, almost 10% of patients with previously validated bidirectional block exhibited arrhythmia recurrences (2,3).
Complications following isthmus ablation are very rare. Atrioventricular block is the most frequent complication (0.2%), though this risk can be minimised by avoiding lesion delivery in the septal part of the cavotricuspid isthmus.
Figure 1. Ablation of typical isthmus dependent flutter 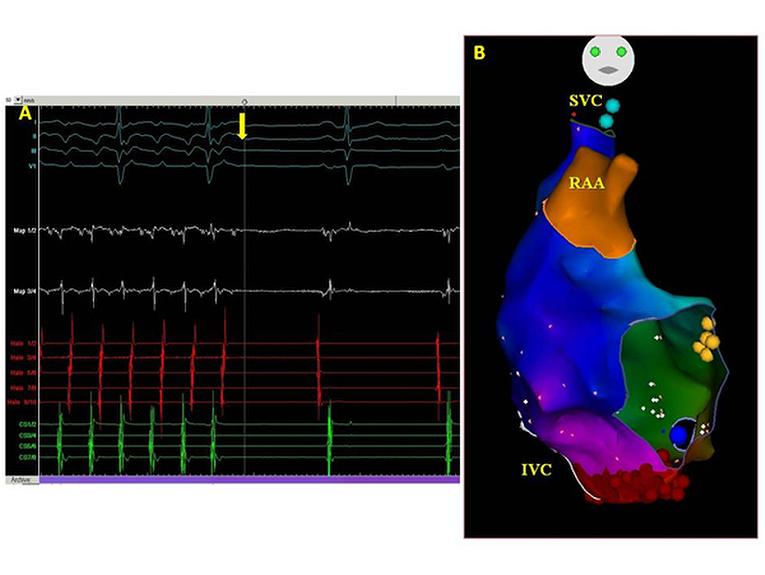
Figure legend:
(Α) Typical atrial flutter is terminated during ablation and converted to sinus rhythm (yellow vertical arrow).
(Β) Three dimensional imaging of the anatomy of the right atrium, the activation mapping during atrial flutter and the linear lesion deployed. Anatomic landmarks demarcated in anteroposterior projection include the superior vena cava (SVC) the inferior vena cava (IVC), the right atrial appendage (RAA), the tricuspid valve annulus, the coronary sinus os (blue dot) and the area where His electrogram is recorded (yellow dots). Lesions are tagged with red dots and form a continuous line extending from the tricuspid valve annulus to the inferior vena cava.
C) Recommendations
Catheter ablation as first line treatment (Class I) for the management of patients with cavotricuspid isthmus dependent flutter (4).
Dofetilide as pharmacological treatment for prevention of recurrent episodes of atrial flutter (Class IIa), while administration of other antiarrhythmic agents such as propafenone, flecainide, amiodarone, sotalol is rather not indicated (Class IIb).
2- Atrioventricular node reentrant tachycardia
A) Presentation
Atrioventricular node reentrant tachycardia is the most frequent paroxysmal tachycardia. The pathophysiological mechanism of this tachyarrhythmia relies on the coexistence of two discrete functional pathways in the atrioventricular node with diverse electrophysiological properties: the slow pathway (slow conduction and short refractory period) and the fast pathway (fast conduction but prolonged refractory period). Apart from the typical AVNRT (slow-fast), atypical AVNRT may also occur (fast-slow και slow-slow) (5).
B) Technique
The target site aimed during AVNRT ablation is the slow and not the fast pathway of the atrioventricular node, since ablation of the slow pathway is related with significantly lower rate of complete heart block as compared to ablation of the fast pathway (6). The slow pathway may be identified based on anatomical and/or electrophysiological criteria. In everyday clinical practice, the most popular implicated strategy is a hybrid of the anatomical and the electrogram-based approach, where usual anatomical sites of slow pathway localisation are visited, searching for target electrograms such as fractionated atrial electrogram combined with a high ventricular to atrial electrogram amplitude ratio (7). Usual sites of succesful slow pathway ablation are the zone between the coronary sinus os and the tricusid valve annulus, the coronary sinus os per se and the area located anterior and caudal to the coronary sinus os. Lesion delivery superior (cranial) to the level of the coronary sinus roof (cranial) should be averted to minimise the associated risk of atrioventricular block. The occurence of junctional rhythm during ablation is indicative of a succesful ablation site (8).
Catheter ablation has earned its evidence-based credentials to be regarded as a safe and effective treatment for atrioventricular node reentrant tachycardia. Recurrence rates following successful slow pathway ablation range from 3% to 7% (9-11). As previously reported, the major procedural complication is atrioventricular block, potentially requiring pacemaker implantation, with an estimated incidence of 1% (12). However, it should be noted that this complication can be reduced further if physicians performing ablations adopt precautions and measures known to prevent atrioventricular block such as strict avoidance of high risk zones, meticulous monitoring of retrograde junctional conduction and immediate termination of lesion delivery in case of retrograde block or even conduction delay.
C) Recommendations
Catheter ablation is the preferred therapy for the management of patients with AVNRT (Class I indication), especially in those with poorly tolerated or recurrent symptomatic AVNRT or in those who desire complete control of their arrhythmia.
3- Accessory pathway (AP)-related tachycardias (WPW syndrome)
A) Presentation
Accessory pathways are extranodal atrioventricular connections which may be implicated in the mechanism of related tachyarrhythmias, either directly (reciprocating tachycardias) or indirectly (bystander participation in supraventricular tachycardias such as atrial fibrillation, atrial tachycardia or AVNRT). The most common AP-related tachycardia is atrioventricular reentry tachycardia (AVRT), a well-defined macroreentry with the bypass tract and the normal atrioventricular conduction system serving as the antegrade or the retrograde limb of the circuit. AVRT is defined as “orthodromic” when the wavefront propagates from the atria to the ventricles via the normal conduction system, or “antidromic” if the bypass tract is used as the antegrade limb. It should be emphasised that orthodromic AVRT may occur in patients without overt preexcitation on surface ECG, in case the accessory pathway possesses only retrograde conduction properties (concealed AP).
B) Technique
In all patients with AP-related tachycardias the treatment of choice is catheter ablation of the AP. Location of the AP based on specific electrophysiological criteria and subsequent lesion delivery results in elimination of preexcitation (Figure 2). The reported success rate of AP ablation is about 95%, with the highest percentages reported in left lateral Aps (13-15). On the other hand, the procedure is more demanding in patients with multiple APs. The left free wall bypass tracts can be ablated either retrogradely (femoral artery access - transaortic approach) or via transeptal access, mainly depending on a physician’s preference. The complication rate with catheter ablation of AP rises to 0.6% and is related to the location of the AP and its distance from the atrioventricular node (16).
Figure 2. Catheter ablation of accessory pathway
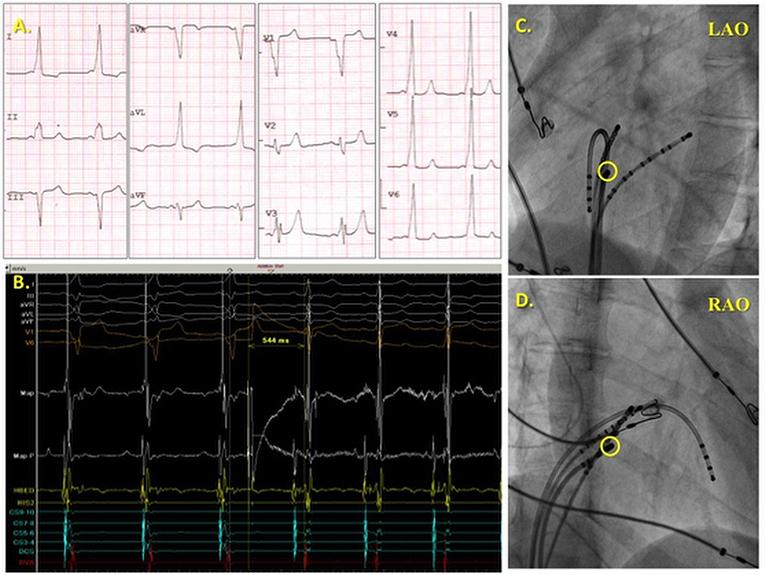
Figure legend :
(Α) The polarity of the delta wave on the surface ECG is suggestive of a right midseptal localisation of the AP.
(B) Ablation is performed during sinus rhythm and 0.5 sec after the onset of radiofrequency energy delivery. Overt preexcitation is eliminated, QRS duration is shortened, while the atrial and ventricular electrograms get separated. (C, D) Fluoroscopic view of the site of succesful AP ablation in left anterior oblique (LAO) and right anterior oblique (RAO) projection located in the midseptum in close proximity to the His catheter.
C) Recommendations
Catheter ablation is the preferred treatment (Class I recommendation) in all patients with WPW syndrome (overt preexcitation and tachyarrhythmias).
4- Focal atrial tachycardias
A) Presentation
Focal atrial tachycardia is the least common type of supraventricular tachycardias and is encountered in 10 to 15% of patients subjected to electrophysiologic study. It is characterised by rythmical generation of impulses either from a discrete focus or from a microreentry circuit, centrifugal propagation and subsequent atrial activation. In cases with one to one atrioventricular conduction, focal atrial tachycardias usually present as long RP tachycardias. Analysis of the P wave morphology using proposed algorithms may prove useful for the identification of the potential site of origin of the tachycardia in 93% of cases (17).
B) Technique
Ablation of focal atrial tachycardias is facilitated by electroanatomical mapping systems which enable non-fluoroscopic navigation of the ablation catheter, formation of the three-dimensional anatomical model of the atrium, activation mapping of the atrial tachycardia, delineation of the underlying mechanism and identification of the site of origin. Apart from satisfying the criterion of earliest activation during tachycardia, target sites usually display a typically fractionated electrogram, prolonged duration and occasionally presystolic activity. The reported acute procedural success rates of atrial tachycardia abation range from 69 to 100% in several patient series, with a recurrence rate of about 7% (18,19).
In case of focal atrial tachycardia, an initial pharmacological management is attempted usually with beta-blockers or calcium channel blockers. However, catheter abation is preferred in patients with drug-refractory, or incessant atrial tachycardias, specifically in the subgroup of patients with tachycardia induced cardiomyopathy.
C) Recommendations
Catheter ablation is the preferred treatment (Class I recommendation) in recurrent symptomatic atrial tachycardias, asymptomatic or symptomatic incessant atrial tachycardias.
Conclusions
Low procedural complication rates as well as high efficacy rates have made catheter ablation the treatment of choice for the majority of patients with supraventricular tachycardias.
In the future, the development and evolution of associated three dimensional electroanatomical mapping systems may further improve the invasive management of patients with supraventricular tachycardias.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.