Background
There is a good relationship between home blood pressure monitoring and cardiovascular prognosis however less evidence supports use clinical decision making. In Spain at least, there are still many cardiologists who give more importance to office blood pressure (OBP) measurements than to HBPM results. This review exposes the reproducibility of this technique, as well as correlation of HBPM with organ damage and long term prognosis.
I - Advantages
The measurement of home blood pressure may circumvent a number of observer errors related to measurements in the physician’s office which are subject to:
- Failure to properly prepare the patient
- Equipment and layout problems - equipment should be properly calibrated and validated
- Miscuffing - the use of a blood pressure cuff that is too large or, more often, too small for the patient’s arm.
- Digit preference - many physicians round off the blood pressure to the nearest 5 or 10 mm Hg
- Deflating the cuff too rapidly
- Discrepancies between observers - Interaction of the doctor (or nurse) with the patient during the measurement which is the most important cause of error (1)
Ayman and Goldshine (2) were the first to report in 1940 that home blood pressure was less reliable than OBP using HBPM. Nevertheless, this issue could not be adequately addressed until ambulatory blood pressure monitoring (ABPM) with full automatic devices was introduced (3). Superiority of home blood pressure monitoring regarding certain patient outcomes has been made more pressing in the past two decades. Because it offers better correlations with the risk of cardiovascular mortality and target organ damage, the information obtained from home and ambulatory methods reflects more accurately the patient’s risk of future cardiovascular events than does OBP.
Better prognosis
A) Cardiovascular mortality
HBPM and ABPM can avoid office-related blood pressure measurement problems and thus put forth information that reflects more accurately the patient’s risk of future cardiovascular events (4,5). In a number of studies, prognostic significance of home systolic BP (SBP) was demonstrated.
- Only home systolic BP (SBP) had a significant relation to the risk of cardiovascular mortality: Starting in 1987, Ohkubo and colleagues assembled a cohort of 1,789 subjects from the rural Japanese community of Ohasama, and compared the prognostic significance of home and office BP measurements. The screening OBP consisted of two measurements by a health-care professional, whereas the home pressures were made up of a morning home BP measurement every day for 4 weeks, with a mean of over 20 measurements collected per patient. The home BP values were analysed as both the average of all measurements per subject at home and the average of the initial two measurements at home. The mean follow-up duration was 6.6 years.
Only home systolic BP (SBP) had a significant relation to the risk of cardiovascular mortality, with a 1 mm Hg rise in home SBP conferring an increased risk of 2.1%. This result supported the assertion that multiple home BP measurements are better able to predict cardiovascular mortality than clinic-based BP measurement (6). - Significant and independent relationship between cardiovascular mortality and pulse pressure: A subsequent study of the same Ohasama cohort demonstrated the significant and independent relationship between cardiovascular mortality and pulse pressure as assessed by home BP monitoring (7), a relationship that had been previously established for clinic-based measurements of BP (8)
B) Target organ damage
Bliziotis et al performed a review and meta-analysis of studies investigating the association of HBPM with target organ damage. A PubMed and Cochrane Library search (1950–2011) pulled 23 studies reporting comparative data of home BP versus ambulatory and/or office measurements and its association with several indices of target organ damage.
- Fourteen studies (n = 2485) assessing echocardiographic left ventricular mass index (LVMI) showed similar correlations with HBPM as with ABPM and superior to office measurements.
- Four studies assessing carotid intima–media thickness, three assessing pulse wave velocity and two assessing urinary protein excretion showed no difference in pooled correlation coefficients with home versus office BP measurements. With all the measurement methods SBP was more closely associated with target organ damage than DBP.
- Ward et al conducted another systematic review and meta-analysis of prospective studies of home BP. They identified eight studies with 17,698 participants. The conclusion was that home BP remained a significant predictor of cardiovascular mortality and cardiovascular events after adjusting for OBP suggesting it is an important prognostic variable over and above that of office BP.
Modified from Hara et al. (9)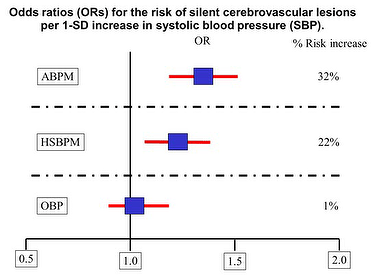
Less medication use
The use of HBPM for adjusting antihypertensive drug treatment is the object of scarce scientific evidence. The THOP trial however did aim to determine whether or not long-term antihypertensive treatment based on HBPM might be more beneficial to the patient than treatment based on OBP. After a 1-month run-in period, eligible hypertensive patients were randomised into two groups. In one group antihypertensive treatment was guided by the diastolic OBP as an average of three sitting readings obtained by a doctor in the office using a sphygmomanometer and, in the other group, antihypertensive treatment was guided by the diastolic home BP as an average of all 42 sitting readings (3 morning and 3 evening for 7 consecutive days prior to the patient’s visit to the doctor). The patients used the Omron HEM-705CP device (Omron Inc., Kyoto, Japan). Regardless of randomisation, both home and office BP were measured in all patients at each visit. After randomisation, the same standardised stepwise treatment regimen was applied in both groups to reach the same target diastolic BP (80 mm Hg to 89 mm Hg).
Four hundred (66%) of the 606 enrolled patients met the entry criteria and were randomised either to office BP (n=197) or home BP (n= 203). At baseline, both the office and home BP groups had similar characteristics and BP values. The median follow-up time was 350 days. Office, home, and ambulatory BP values significantly decreased after randomisation in both treatment groups.
After 6 months of treatment, the decreases in BP were similar in the two randomised groups.
Thereafter BP reductions became consistently and significantly greater in the office BP patients than in the home BP patients.
HBPM allowed the discontinuation of antihypertensive drugs in twice as many patients and thus helped to identify patients with white-coat hypertension. More patients in the HBPM group than in the OBP group were able to permanently stop antihypertensive treatment, but the opposite trend was observed for patients proceeding to multiple drug treatment. In both treatment groups there were similar significant decreases in electrocardiographic indexes of left ventricular mass.
From the above, authors concluded that adjustment of antihypertensive treatment based on HBPM instead of OBP led to:
- Less intensive drug treatment, but also to less BP control for the long-term with no differences in general well-being and electrocardiographic indexes of left ventricular mass
- Discontinuation of antihypertensive drugs in twice as many patients.
The findings of the THOP trial (10) do not demonstrate that HBPM might be a better guide to antihypertensive drug treatment than conventional OBP measurement but show some comparative benefits.
In the same way, the HOMERUS trial (Home Versus Office Measurement, Reduction of Unnecessary Treatment Study) showed that HBPM leads to less medication use than OBP measurement without leading to significant differences in OBP values or target organ damage (11). BP values, however, remain slightly elevated for the HBPM group. Since current clinical guidelines strongly recommended avoid deep decreases of BP (12), this may be an argument favoring HBPM use. Nevertheless, some trials have found the contrary conclusion (13).
Reproducibility
The reproducibility of various methods of pressure measurements is challenged by the fact that each tends to define only one aspect of a person's BP:
- A central point: Average ABPM may reflect a central point around which pressure varies over the course of a day.
- An extended period: HBPM reflects an average level of BP over an extended period (usually, 1 week), when measurements are made in a a similar environment.
- A singular circumstance: Clinician-measured pressure reflects a point measure of pressure under a singularly peculiar circumstance.
- Many versus fewer measurements: There are more ABPM measurements than clinic measurements. This fact may make the ambulatory average more reproducible, since the greater number of measurements makes it less sensitive to extreme single readings and is also likely to be independent of factors that increase measurement error, such as measurement anxiety, observer-subject interaction and digit preference.
- Diversity of time points: ABPM provides BP information at many time points on a particular day during unrestricted routine daily activities, whereas HBPM provides high amounts of BP information obtained under fixed times and conditions over a long period of time; thus, it could be considered that the mean values of HBPM are more stable, and the reproducibility are higher (14).
- Possibility of repeated measurements: HBPM is simple to repeat and track, ABPM is not suitable for repeated measurements. It has been reported that HBPM yields minimal alerting effects and novelty effects, good reproducibility of BP levels, no regression to the mean and a minimal placebo effect (15).
- Sensitivity: HBPM can distinguish small but significant serial changes in BP (16).
Historically, the reproducibility of home, clinic, and ambulatory BP was first evaluated by James et al as far as 1988, although previous evidence suggested that among hypertensive patients these may stay about the same or drop over time (17). Authors compared a group of 13 untreated mildly hypertensive subjects with a group of 14 normotensive subjects. Each subject had two sets of daily ambulatory recordings, HBPM readings over 6 days, and clinic measurements taken two weeks apart. Results showed that:
- Particularity of clinic SBP: There was no consistent average change in either group in the ambulatory or home pressures nor clinic DBP with the exception of the clinic SBP of the hypertensive patients which fell by 6 mm Hg
- Uniformity of results across methods: Test-retest correlations were similar across the methods, indicating similar levels of reliability, in other words the distributions of pressure averages (SDP and DBP) for each method of measurement remained relatively stable over the 2 weeks in this sample.
- Reproducibility as good or better: ABPM tended to correlate better with HBPM than with clinician-measured pressures; therefore the reproducibility of HBSPM could be as good as that of ABPM or clinic BP measurements (18).
BP readings fall with multiple readings, the extent of which varies according to the interval between successive readings although usually the differences are quite small (19-21). Nonetheless, the differences between triplicates have been sufficient in at least one study for the diagnosis of “hypertension” to be made more frequently with the first than with the mean of the 2nd and 3rd measures (22). On the other hand, some of the guidelines recommend discarding the higher measurements that are often measured initially, but this refinement had no impact in explanatory modelling of cardiovascular risk or organ damage (23).
Precision in estimating cardiovascular risk can be expected to increase with the number of measurements for estimation of BP.
- Averaging more readings preferable, best agreement between ABPM and HBPM morning readings: Niiranen et al. found that the most precise predictions were achieved by including all values of duplicates measured twice per day over 7 days, though the measurements made over the first 3 days were more influential than those made later (24). Other authors agreed that by averaging more readings, the average HBPM and its variability are reduced and the prognostic ability improved (25). Finally, the best agreement between ABPM and HBPM appeared to be in the morning between the first HBPM of the day and the mean of the 4 observations taken in the second hour after the patient had wakened (26).
- Only two days to show superiority of HBPM over OBP: Stergiou et al in 1998 (27) conducted a study to determine the minimum number of measurements of HBPM necessary to provide the maximum clinically important benefit. Hypertensive patients were randomly allocated to make HBPM for 2 weeks (6 work days, duplicate measurements, twice daily) or 24h ABPM. OBP was measured at the beginning and the end of the study. The reproducibility of HBPM was quantified using test–re-test correlations and the SD of differences between average HBP values of different days in a group of 189 patients. Average HBPM was lower than average OBP and higher than 24h ABPM. There was no difference between HBPM and daytime ABPM. On day 1 HBPM was higher than it was on each of days 2–6, with no difference among days 2–6. When data for the initial day for monitoring of HBPM were excluded from analysis, average HBP was reduced. Only a modest improvement in the reliability of HBPM on day 2 was achieved by averaging more blood pressure readings taken on following days. Only two monitoring days were needed for the reproducibility of HBPM to be superior to that of OBP.
Most comparisons between HBSPM and ABPM have been made in order to detect isolated clinic hypertension (white coat hypertension).
- Masked hypertension uncovered more often with HBPM‐office pairings,: Viera et al (29) examined 1‐week reproducibility of masked hypertension by HBPM and ABPM. They recruited 420 untreated adults, with recent clinic BP between 120/80 and 149/95 mmHg.
Based on office‐awake ABPM pairings, prevalence was 44 and 43%, with an agreement of 71%.
Based on HBPM‐office pairings, prevalence when considering the 24‐h average was higher, with 50 and 48% and agreement of 82%.
On the other hand, less attention has been paid to reproducibility over time of OBP and HBPM.
- Reproducibility of home blood pressure over time is superior to that of screening blood pressure: Sakuma et al conducted a study on the reproducibility of HBPM over a 1‐year period (29). A total of 136 untreated subjects without cardiovascular complications were analysed in the study. The correlations between the first and second BP measurements of the subjects were significantly higher for the HBPM than for the screening BP measurements. Mean differences between the first and second HBPM were significantly smaller than those for the screening blood pressure, suggesting that the reproducibility of home blood pressure over time is superior to that of screening blood pressure.
Conclusions
Home blood pressure monitoring is an inexpensive and convenient method to measure blood pressure in an environment familiar to the patient.
The reproducibility of home blood pressure monitoring is comparable to, or even better, than traditional office based blood pressure measurements and it overcomes some biases in office based readings such as digit preference and observer bias.
Much evidence has accumulated that shows that HBP is able to predict hypertensive target-organ damage and a prognosis of cardiovascular disease more effectively than OBP and nearly as well as ABPM.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.