Background
Following new guidelines concerning the use of devices in patients with congestive heart failure (1), cardiac implantable electronic devices (CIEDs) - and implantable cardioverter defibrillators - especially have grown in use. Unfortunately, this trend has been accompanied by an increase in infection rate, probably due to an increase in comorbidities. A recent analysis of US data (2) showed that infection rate grew from 1.61% in 1993 to 2.41% in 2008, possibly due to two factors: ageing of population and increased use of more complex devices. Several studies (3-4) have found that the most important risk factors for infection are re-intervention, with device replacement increasing with ageing of population, and use of dual and triple chamber devices, increased in the last years.
Early diagnosis and correct treatment of this situation is of great importance: if the local infection is not correctly treated and bacteraemia or device endocarditis is present, in-hospital mortality can rise from 5% to 29% (5).
I - Diagnosis: Transoesophageal echocardiography and bacterial culture, but waste no time
A patient that comes to our attention because of changes to the aspect of the CIED’s pocket: colour, volume, skin adherence to CIED; figure 1A, 1B and 1C are cases from our practive we offer for your review, with or without CIED exposure, should be carefully investigated for signs of CIED infection, while making no attempt to drain pocket, because this manoeuvre itself can result in device infection.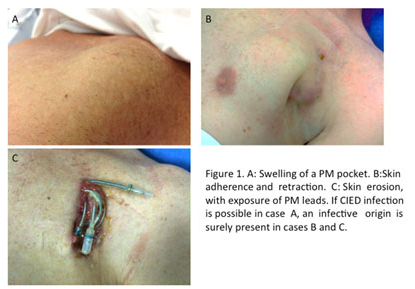
Until some years ago, it was unclear if skin lesions of the pacemaker pocket were always related to infections, but several studies have demonstrated that local signs of inflammation, in at least 75% of cases, are related to infection (6), and in the remaining cases, proofs of bacterial colonisation could not be excluded. If infection remains localised to the CIED pocket, the patient will not present with systemic signs of infection. Indeed, fever, chills and general malaise relate to the diffusion of the infective process to the blood stream. In the early phases of this process, biochemical examinations (white blood cells count, C-reactive protein, erythrocyte sedimentation rate) could remain within normal range, but culture of eventually extracted leads could result be positive in up to 88% of patients (7).
Transoesophageal echocardiography (TEE) remains the most important tool to identify the presence of bacterial vegetations along the leads or over the valvular leaflets (8,9) and therefore should always be performed in cases of suspected or confirmed infection. Transoesophageal echocardiography is the best technique to evaluate the dimension of the vegetations dimension, since this parameter is of great importance when deciding on the best approach to extract the infected leads (10).
Recently, several studies have underscored the usefulness of Fluorine 18 Positron Emission Tomography/Computed Tomography (FDG 18 PET/TC) in the identification of CIED infection (11-12). This technique can identify tissues with high glucose uptake rates, as “active” leucocytes or tumor cells. Fluorine 18 Positron Emission Tomography/Computed Tomography is not only able to give a response of “inflammation or not” but it can also provide semi-quantitative information regarding the extent and the severity of the inflammatory process and on possible foci of infection that gave rise to the CIED infection (Fig. 2).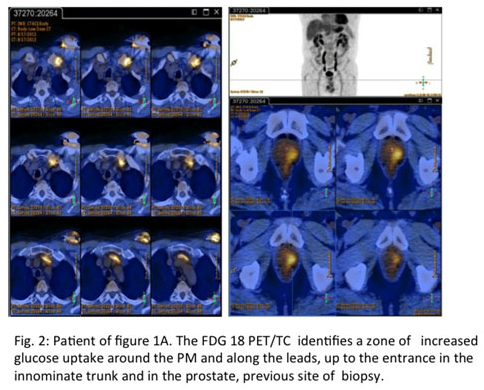
The main point that every cardiologist should keep well fixed in mind whenever he or she deals with a patients with suspected CIED infection is to reach a diagnosis as soon as possible, because the time spent in obtaining a diagnosis could impact heavily on the patient’s prognosis (7).
II - Treatment : Only removal of the complete pacing/defibrillation system can cure patient
Table I reports the current guidelines (13) on treatment of patients with definite CIED infection. It is clear that every CIED infection should no longer be merely treated with antibiotics. Only removal of the COMPLETE pacing/defibrillation system (PM/ICD) can really CURE the patient.
Table 1: Complete device and lead removal
Class of recommendationSituationLevel of Evidence1Recommended for all patients with definite CIEDs infection, as evidenced by valvular and/or lead endocarditis or sepsisA.1Recommended for all patients with CIED pocket infection as evidenced by abscess formation, device erosion, skin adherence, or chronic draining sinus without clinically evident involvement of the transvenous portion of the lead system.B1Recommended for all patients with valvular endocarditis without definite involvement of the lead(s) and/or device.B1Recommended for patient with occult staphycoloccal bacteraemia.B2aIs reasonable in patients with persistent occult Gram-negative bacteraemia despite appropriate antibiotic therapy.B
Despite these clear guidelines, a recent European survey showed that 43.5% of European interviewed centres perform pacing system extraction in case of local infection of the implanted CIED in comparison to the 95% of centres that perform pacing system removal in cases with systemic signs of infection or with valvular/lead endocarditis (14). This behaviour should be discouraged, because earlier complete system removal results in improved survival, as previously reported (5).
Even though lead extraction remains a complex and potentially dangerous procedure, results from large volume centres demonstrate that lead extraction is feasible and safe in a large majority of patients, reaching an approximate success rate of 99% and with a rate of fatal complications lower than 0.5%(15-16).
Benefits of lead extraction in cases of infection strongly outscore procedural risks. In a recent paper(17), Maytin and coll. found that the mortality rate at 30 days, 3 months and 1 year respectively were 2.1%, 4.2% and 8.4%. These data should strongly encourage the use of this procedure, because the mortality figures of CIED infections not correctly treated could reach value as high as 11% at 30 days or 17% at 1 year according to several studies (18-19).
Guidelines(13) also suggest the appropriate timing of reimplantation: these indications are reported in Table II (modified from reference 11).
Class of recommendationIndicationLevel of Evidence
IEach patient should be carefully evaluated to determine if there is a continued need for a new CIEDIThe replacement device implantation should not be ipsilateral to the extraction site Ia CIIaIn patients without vegetations, but positive lead tip cultures, a new CIED can be implanted if there are no more signs of systemic infection and the blood cultures drawn within 24 hours of CIED system removal remain negative for at least 72 hours.In patients without vegetations, but preoperative positive blood cultures, a new CIED can be implanted if there are no more signs of systemic infection and the blood cultures drawn within 24 hours of CIED system removal remain negative for at least 72 hoursCCIIaIn patients without vegetations, but preoperative sepsis and positive blood cultures, a new CIED can be implanted if there are no more signs of systemic infection and the blood cultures drawn within 24 hours of CIED system removal remain negative for at least 72 hours.CIIaIn patients with vegetations it is reasonable to delay CIED reimplantation for at least 14 days.C
The correct timing of reimplanting is crucial, in order to reduce as much as possible a new infection, that could compromise the possibility of a endovascular access for an eventual new device.
Conclusions
Infection of implanted CIED represents a very severe situation. For these patients, early diagnosis can make a great difference in terms of survival. Antibiotics and conservative approach (i.e. without CIED system removal) are not sufficient to correctly and definitively treat this condition. For these reasons, current guidelines recommend lead extraction and CIED removal. This procedure could significantly reduce mortality in these patients who – incorrectly diagnosed and treated – maintain a mortality rate as high as 17% at 1 year. In experienced centres, endovascular lead extraction is highly effective and safe, with rates of perioperative mortality lower than 1%.


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.