 Background
Background
Cardiovascular disease in women, their specific symptoms in presenting myocardial infarction and the Women at Heart initiative have been brought to you in a previous volume of the e-Journal, in 2006. Since, the ESC/EACPR 2007 guidelines have exposed the misleading or incomplete issues regarding this category of risk - being female- in a dedicated a section (1) and among issues raised were:
- Cardiovascular disease (CVD) in women appears ten years later than in men. We now know that despite this fact the total number of deaths due to major cardiovascular events in women (55%) is higher than in men (43%).
- Obesity, metabolic syndrome and diabetes are more prevalent in middle-aged and elderly women who appear to carry a greater risk of cardiovascular death.
- Women are at a disadvantage at all stages of evolution of cardiovascular disease.
Taken together, these findings indicate that the Heart Score and/or other classical charts are not fully suited to quantify risk in women. New tools, whether methods or charts, are needed for better evaluation of women's specific cardiovascular risk, especially at its early stages.
Reynolds Risk Score
- Lower HDL cholesterol values are associated with higher cardiovascular risk. To determine HDL cholesterol, testing can be carried out on a routine basis. Low HDL is also a common characteristic of obesity, metabolic syndrome and diabetes mellitus thus it is reasonable to think it contributes highly to women’s cardiovascular risk.
- From a physio-pathological point of view, high sensitivity CRP is valuable even though it is not routinely tested in laboratories and is more expensive than HDL cholesterol testing. High sensitivity CRP nevertheless, is directly linked to obesity, inflammation and atherosclerosis. Furthermore, in establishing cardiovascular disease CRP cut-off values are different in women than in men. (4,5)
- The Reynolds risk chart also includes death in first degree relatives under the age of 60 as well as the more usual parameters which are smoking status, total cholesterol, age and systolic blood pressure. Here you will find a useful, free version on line. (3)
Although data published in the last five years are numerous, results obtained with the chart remain a matter of controversy.(6) The Reynolds risk score can, however, be validated with classical charts such as Heart Score, Framingham, and ATP III. This added step may be useful reclassifying the woman with risk determined by classical charts as intermediate, into a more specific category: low or high risk.
Adiponectin
Epicardial adipose tissue may be an important regulator of patho-physiological processes contributing to coronary artery diseases (CAD), through local production of various cytokines and adipocytokines. (7,8)
Body mass index, waist circumference and waist to hip ratio can be used to evaluate obesity. However, BMI is a poor measure of body fat in the over age 65 population mainly, due to sarcopenic obesity, that is due to age-related reduction in skeletal muscle mass. Waist circumference and waist to hip ratio are the preferred methods in this population. Furthermore, the values of the parameters listed above have cut-off values that differ by race, sex, and other factors.
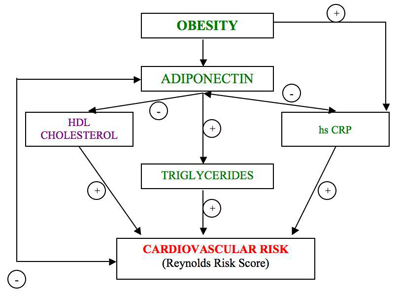
It is believed that adipose tissue secretes adipocytokines which influence cardiovascular risk, of which adiponectin, first discovered over twenty years ago, is a member. Adiponectin is secreted by white adipose tissue (as opposed to brown) and levels are low in obese people. (7,8) Indeed, levels of the hormone are inversely correlated with body fat percentage in adults. Levels of adiponectin are also influenced by smoking, age, and sex. There are added correlations with risk factors such as total cholesterol, HDL cholesterol as well as inflammatory markers, hs protein C and interleukins (9).
Adiponectin is likely to play an important role in the interplay between metabolic changes and cardiovascular risk, however the central question is whether levels - high or low - indicate protection against atherosclerosis and cardiovascular disease. In women without cardiovascular disease, high plasma adiponectin levels are correlated with low cardiovascular risk. In women with cardiovascular diseases however, high plasma levels reflect a high risk. (10,11)
Adiponectin and the Reynolds risk score
We attempted to establish whether there is a link between adiponectin plasma levels and the Reynolds Risk Score in women with metabolic syndrome but without any major cardiovascular event (12). Findings showed that women with metabolic syndrome have a lower level of adiponectin compared to women without syndrome thus plasma adiponectin alone may be of little value in the diagnosis of metabolic syndrome. Unfortunately, no correlation could be established between plasma adiponectin levels and RRS.
These findings are paradoxical. However, they might be explained by the fact that adiponectin homeostasis is differently regulated during chronic inflammatory states, such as established CVD, which increase adiponectin concentrations independently of adipose tissue regulatory mechanisms.
Patients with rheumatoid arthritis for instance, another chronic inflammatory condition, have higher adiponectin levels and increased inflammatory status compared with healthy controls.
Further studies are needed to confirm the value of RRS in women and to elucidate the role of adiponectin in these processes of atherosclerosis. Nevertheless, a very recent case-cohort sample of the multi-ethnic Women's Health Initiative Observational Cohort with 1722 cases of major CVD and a random subcohort of 1994 women without prior CVD demonstrated that the Reynolds Risk Score is better calibrated than the Framingham-based models to predict global cardiovascular risk (13). Corroborating all data, a theoretical mechanism of adiponectin and cardiovascular risk linked RRS was part of Author's PhD thesis. (Fig. 1)
Figure 1: The Reynolds Risk Score, designed by Author.
Conclusion:


 Our mission: To reduce the burden of cardiovascular disease.
Our mission: To reduce the burden of cardiovascular disease.